Review Article - (2018) Volume 8, Issue 5
Neuroimaging Advances in Preclinical Alzheimers disease
- Corresponding Authors:
- Yue Huang, MD, PhD
Brain Bank at China National Clinical Research Center for Neurological Diseases, Beijing, P. R. China
Fang Liu
Department of Neurology, the First Hospital of Tsinghua University, Beijing, P. R. China
Abstract
Alzheimer’s disease (AD) is considered as a continuously pathological continuum. The AD pathophysiological process begins decades before the emergence of clinical symptoms. Recently, due to the advanced neuroimaging techniques and biochemical tests, various biomarkers are gradually identified, providing the ability to detect the evidence of AD pathology in the preclinical stage and further intervene the process of disease. Multimodal magnetic resonance imaging (MRI), with relatively non-invasive and economic benefits, is of great values to promote the clinical application. Therefore, researches involving brain structural and functional alterations in preclinical AD are summarized in this review.
Keywords
Alzheimer’s disease, Preclinical, Magnetic resonance Imaging, Neuroimaging
Introduction
Alzheimer’s disease (AD), characterized by progressive deficits in memory and other cognitive fields, has a long asymptomatic phase during which AD-related pathophysiological abnormalities, such as amyloid-β (Aβ) deposition, neurofibrillary tangles (NFTs) formation and proliferation of glial cells, have been apparent [1,2]. Given lack of effective treatments and failure of numerous clinical trials at the stage of dementia, the preclinical phase of AD may provide a crucial opportunity for postponing and even preventing the process of the disease.
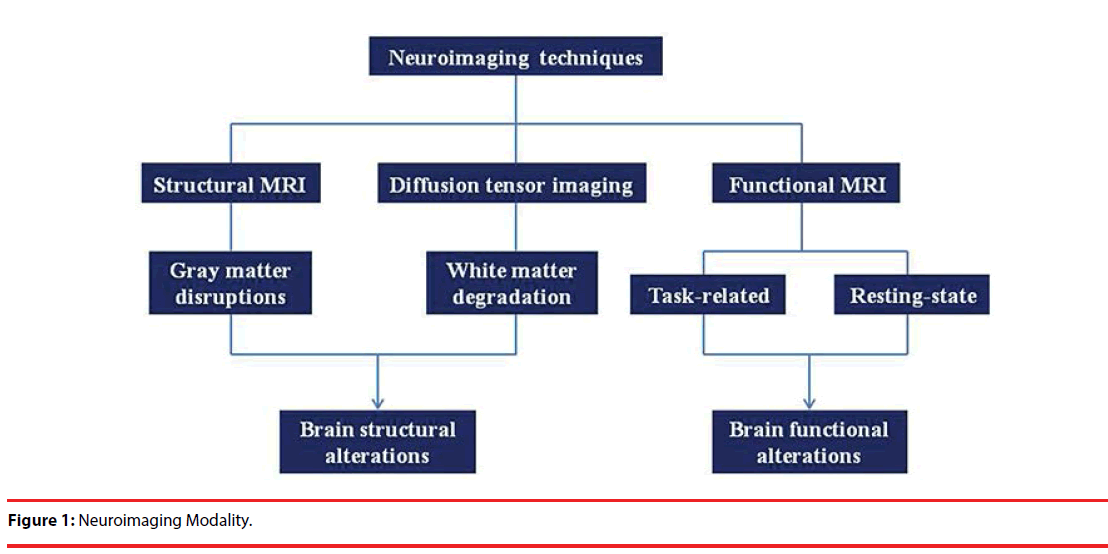
Due to the absence of specific clinical phenotypes and a lower sensitivity of the current neuropsychological scales in identifying potential individuals in presymptomatic AD, the application of pathological biomarkers stemmed from cerebrospinal fluid (CSF) and positron emission tomography (PET) is of great importance to achieve accurate diagnosis in vivo before the appearance of AD clinical symptoms. Reduced levels of Aβ42 combined with raised concentrations of tau in CSF and alternative Aβ and tau deposition in brain detected by PET imaging would provide relatively objective information reflecting AD-related pathology [3,4]. However, the above-mentioned biomarkers have some defects in utility because of their invasiveness and radioactivity. Recently, the advances of multiple neuroimaging techniques, such as structural MRI (sMRI), functional MRI (fMRI), diffusion tensor imaging (DTI), have offered a promising prospect that allows noninvasively investigating abnormalities of brain structure and spontaneous functional activities in early AD [5]. Additionally, previous studies have investigated that AD is a disconnection syndrome with multiple etiologies and complex mechanisms [6,7]. Therefore, a systemlevel research based on brain anatomical and functional connectome is beneficial to gain an insight into the changes of whole-brain connectivities [8]. Here, we will introduce the conceptual framework of preclinical AD over the past decade. Then, we further elucidate specific neuroimaging properties in the presymptomatic stage of AD.
̢̻̉ Criteria for preclinical AD
Dubois et al. initially proposed the definition of preclinical AD in 2007, which means a long asymptomatic phase from the appearance of brain pathophysiological changes to the onset of subtle clinical symptoms [9]. Individuals with the evidence of Alzheimer’s pathologies have high likelihood to develop clinical AD. Subsequently, in 2010, the international working group (IWG) further distinguished two preclinical states of AD, including the presymptomatic state and the asymptomatic at risk state [10]. The term “presymptomatic state” is designated for carriers with an autosomal dominant monogenic AD mutation who will inevitably present AD clinical symptoms during their lifetime. Whereas, cognitively normal individuals with at least one biomarker reflecting pathophysiological features of AD only have the potential to trigger the characteristic clinical phenotype, which is implicated as individuals in asymptomatic at risk state. Additionally, in 2014, researchers further elaborated on the research diagnostic guide for preclinical AD in the revised IWG-2 criteria [4]. It is noteworthy that aforementioned criteria for preclinical AD require the absence of AD clinical symptoms.
Another classification of preclinical AD stages aims at stratifying patients on the basis of multiple biomarkers. Based on the classic biomarker model initially proposed by Jack [11], National Institute on Aging-Alzheimer’s Association (NIAAA) has defined three different preclinical states: cognitively normal subjects with amyloidosis (stage 1), amyloidosis with evidence of neurodegeneration (stage 2), and amyloidosis, neurodegeneration and subtle cognitive decline (stage 3) [1]. This criterion emphasizes that tauopathy is a sign of “downstream” neurodegeneration and Aβ deposition without the emergence of neurodegeneration is sufficient to make a definite diagnosis of AD. In contrast, numerous studies have shown that Aβ load is not in parallels with brain anatomic changes and dysfunction. Moreover, several postmortem studies have confirmed that some individuals with the evidence of Aβ deposition may not display cognitive decline before their death. Therefore, the IWG-2 criteria have further highlighted the coexistence of decreased Aβ and increased total-tau or phosphorylated-tau in CSF for confirming AD pathology [2].
Recently, the AD biomarker model has been gradually challenged [2,12]. Some researchers consider that this model is just suitable for familial AD, while sporadic AD may not abide by the time sequence of various biomarkers [13]. In order to portray the preclinical phase accurately, Dubois et al. redefined the concept of preclinical AD on the basis of the risk dichotomy to progress to clinical AD [2]. Current studies have indicated that the combination of amyloid and tau pathology may be most suitable in stratifying individuals with the highest risk of conversion to AD [14], while individuals exhibit an isolated brain amyloidopathy or tauopathy have relatively lower risk. Taken together, whatever the stage (preclinical, mild cognitive impairment or dementia), the co-occurrence of Aβ and tau could confirm the final diagnosis of AD.
̢̻̉ Brain structural imaging
̢̻̉ Structural MRI
Structural MRI, as a promising neuroimaging technique, has the potential to distinguish individuals with a high likelihood of conversion to AD, monitoring the disease progression and further evaluate the effectiveness of therapeutic intervention [15]. Brain structural abnormalities, characterized by local brain atrophy and disrupted global structural connectivity, have been previously shown in patients with AD. Using structural MRI, numerous studies have reported a significant volume reduction of the medial temporal region, parietal lobe, and posterior cingulate both in AD and MCI [15-17]. Current researches also validate the similarity of spatial distribution in structural changes occurring decades before the onset of AD symptoms [18-21]. The earliest preclinical changes appear to be the entorhinal cortex approximately 8-10 years prior to the clinical symptom onset, followed by the hippocampus and amygdala, indicating that the medial temporal lobe is likely to be the earliest site attacked by Alzheimer’s pathologies [22-24]. In support of this proposal, based on voxel-based morphometry (VBM) and shape analysis of MRI, Tondelli M et al. also confirmed the significant atrophy at baseline in the right medial temporal lobe for those individuals later diagnosed as AD [19]. It is inconsistent with findings in another study that local frontoparietal regions may be initially affected by emerging β-amyloid pathology while effects in the temporal cortex appear later [25]. These discrepancies of abnormal brain regions among different studies are partly explainable by different sample size and analysis strategies used. Additionally, brain structural changes may be affected by the interaction between amyloidosis and tauopathology. For instance, Fortea J et al. proposed that cortical atrophy only occurs in subjects with both Aβ (+) and phosphorylatedtau (+) [26]. Cognitively healthy individuals only with the evidence of amyloidosis have reduced atrophy rates in cortical thickness while those with decreased CSF Aβ values and raised CSF tau levels simultaneously present accelerated atrophy in medial temporal structures, depicting a biphasic trajectory of brain structural changes in preclinical AD [27].
Besides regional brain structural changes associated with worse cognitive performance in specific domains, discrete neuroanatomical networks have widespread interruption of information integration within and between brain regions. Currently, researchers have demonstrated the relationship between disruptions of gray matter network and ADrelated pathology in cognitively normal adults. Tijms, et al. found that lower Aβ42 levels in the CSF could be linearly associated with lower connectivity density at whole brain level, nonlinearly with lower clustering and higher path length values, indicating a reduced efficiency of network organization in preclinical AD [28].
̢̻̉ Diffusion tensor imaging
Diffusion MRI or DTI is another neuroimaging technique mirroring the white matter degradation [29]. Previous studies have manifested widespread white matter disruptions represented by decreased fractional anisotropy (FA), increased mean diffusivity (MD) and increased radial diffusivity (RD) in AD and MCI patients [30-32]. The existence of white matter microstructural changes has also been confirmed in the presymptomatic AD. Molinuevo et al. revealed that cognitively normal individuals with positive Aβ42 had increased axial diffusivity (A×D) in several white matter fiber tracts, such as corpus callosum, corona radiate, superior longitudinal fasciculus, etc., while other diffusion MRI indexes, including fractional anisotropy (FA), mean diffusivity (MD), and radial diffusivity (RD) have no differences [33]. This study demonstrated the subtle loss of axonal myelination with widely preserved white matter integrity in preclinical AD.
Converging evidences have shown that emerging amyloidosis alone is not sufficient to disrupt the brain structural connectivity, while individuals with the evidence of neurodegeneration are able to present alterations of the white matter connectome even without the amyloid pathology [34]. Furthermore, for individuals with both amyloid pathology and neurodegeneration (A+N+), abnormalities in structural network topology are more significant. Previous studies reported that MCI (A+N+) subjects exhibited distinct brain structural connectivity patterns which is in line with those alterations in patients with AD [35]. Similarly, employing DTI combined with graph theory, cognitively normal individuals with A+N+ showed obvious abnormalities in topological properties characterized by longer paths, lower efficiency, increased clustering and modularity compared with subjects only with neurodegenerative evidence [36]. We list changed brain structural patterns of preclinical AD in Table 1.
| Study | Techniques | Subjects | Sample | Measures | During | Main results |
|---|---|---|---|---|---|---|
| Tondelli, et al. [19] | sMRI | CN1 | 148 | Volume | 10 years | 1.Structural brain changes occur years before the onset of clinical symptoms; 2. Subjects later developing AD have significant atrophy at baseline in the right medial temporal lobe. |
| Pegueroles, et al. [27] | sMRI | CN | 98 | Cortical thickness | 2 years | It is a biphasic trajectory of changes in brain structure in preclinical AD. |
| Soldan, et al. [24] | sMRI | CN | 245 | Volume, thickness | 18 years | Not only baseline hippocampus but also entorhinal cortex measures are associated with the time to progress from normal cognition to cognitive impairment independently of cognitive reserve and ApoE-ε4 genotype. |
| Younes, et al. [22] | sMRI | CN | 349 | Volume, surface area | up to 18 years | During preclinical AD, changes in the shape of the entorhinal cortex precede those in the hippocampus and the amygdala. |
| Miller, et al. [20] | sMRI | CN | 349 | Volume, thickness | up to 17 years | 1. Structural markers of the amygdala, hippocampus and entorhinal cortex are significantly different between controls and those with preclinical AD; 2. Entorhinal cortex is more affected in the early onset of the disease than the other structures |
| Miller, et al. [23] | sMRI | CN; preclinical AD; symptomatic AD |
230; 50; 20 |
Volumes, surface area and thickness |
up to 17 years | 1. The earliest changes within the medial temporal is in entorhinal cortex; 2. There is selectivity of neurodegeneration in early AD. |
| Mattsson, et al. [25] | sMRI | CN; AD |
47; 15 |
Volumes | 4 year | Early Aβ pathology may have mild effects on local frontoparietal regions while effects in temporal regions appear later and accelerate. |
| Fortea, et al. [26] | sMRI | CN | 145 | Cortical thickness | / | Pathological cortical thickening is associated with low CSF Aβ, followed by atrophy once CSF p-tau becomes abnormal. |
| Schroeder, et al. [21] | sMRI | CN | 69 | Cortical thickness, volumes, shape, surface area | / | Localized shape measures (hippocampal) and cortical thickness (entorhinal cortical region) may be potential biomarkers of presymptomatic AD. |
| Tijms, et al. [28] | sMRI | CN | 185 | Degree, clustering coefficient, and path length | / | Lower Aβ42 levels can be related to the disruptions of gray matter networks and these relationships were specific to regions, such as medial temporal lobe, precuneus and the middle frontal gyrus. |
| Besson, et al. [18] | sMRI; FDG-PET | CN | 54 | Volume | / | 1. MRI and FDG-PET biomarkers should be used in combination, offering an additive contribution; 2. Aβ and tau-related pathological processes may interact but not necessarily appear in a systematic sequence. |
| Jack, et al. [60] | sMRI; amyloid PET |
CN | 1246 | Hippocampal volume | / | 1.Memory loss and hippocampal atrophy occur at earlier ages than amyloid deposition; 2. Brain structural and cognitive decline are associated with aging but not Aβ deposition. |
| Pereira, et al. [36] | DTI | CN | 357 | Paths, efficiency, clustering, modularity |
2 years | 1. CN with neurodegeneration showed a disrupted network topology characterized by longer paths, lower efficiency, increased clustering and modularity; 2. CN with both amyloid pathology and neurodegeneration showed more significant abnormalities in all global network measures. |
| Molinuevo, et al. [33] | DTI | CN | 19 (Aβ42+); 19 (Aβ42-) |
Axial diffusivity (AxD) | / | Subtle axonal disruptions occurred in preclinical AD, whereas white matter integrity is still widely preserved. |
| Kantarci, et al. [34] | DTI | CN; MCI |
570; 131 |
Fractional anisotropy (FA) | / | Amyloid load alone does not influence white matter integrity without coexistent gray matter neurodegeneration in preclinical AD. |
“/ ” means: the study is not longitudinal.
Table 1: Summary of brain structural changes for preclinical AD based on sMRI and DTI.
̢̻̉ Brain functional imaging
Functional MRI (fMRI), one of the most common imaging techniques, allows to reveal brain functional activities based on the principle of blood oxygenation level dependent (BOLD) [37]. Task-related fMRI can reflect the activation of local brain regions when subjects execute special tasks and accept external stimulus, whereas resting-state fMRI indirectly mirrors neural activity via exploring spontaneously lowfrequency amplitude at rest state. Accumulation of Aβ in the brain might bring about the synaptic dysfunction, leading to functional disconnection and abnormal information communication among multiple brain regions [38]. The progressive disruption in brain area connectivity contributes to subsequent cognitive decline, which is even prior to brain structural changes, such as neuronal apoptosis and atrophy [39,40].
̢̻̉ Task-related functional MRI
Previous studies have investigated that patients with MCI had increased functional activities within medial temporal lobe in compensating for brain structural damages [41-43]. One latest research has also verified the consistent functional activation in hippocampus during the memory encoding task for amyloid-positive asymptomatic subjects [44]. Longitudinally, raised hippocampus activity at baseline is likely to promote Aβ accumulation in brain cortices, followed by further cognitive decline, indicating the close correlation between hippocampus functional activation and AD-related pathology [45]. Furthermore, entorhinal cortex, one of the key components in default mode network (DMN), exhibits pathological aggregation of tau earlier than that in hippocampus and may present the earliest functional alterations [46]. Currently, it has been demonstrated that hippocampal activations and entorhinal deactivations are modulated during an episodic memory task. Nevertheless, amyloid-positive older adults with normal cognition have reduced ability to modulate activity in entorhinal cortex, but not hippocampus, signifying that entorhinal cortex may be the first brain area attacked by Aβ among the DMN regions [46]. This is consistent with findings mentioned earlier via structural MRI. In addition, normally, frontotemporal network connectivity is increased with aging during an incidental episodic encoding task in compensating for the reduced regional activity, further maintaining the performance of episodic memory. However, for subjects with Aβ deposition, they display no changes of functional connectivity in frontotemporal network, but increased regional activities, which is not associated with cognition improvement [47]. From the above observations, Aβ deposition will affect neuronal activity when memory encoding task is executed.
Besides DMN, frontoparietal control regions, associated with cognitive control or working memory, also have the Aβ accumulation even in the elderly [48,49]. Oh et al. found hyperactivation in frontoparietal control regions during the process of working memory, suggesting that Aβ-related hyperactivation is not specific to the episodic memory system but occurs in frontoparietal control regions as well [48]. Furthermore, another study revealed that functional activity in frontoparietal control regions is related to the difficulty of tasks. For higher cognitive control load, Aβ-positive elderly showed reduced task-switching activation in the right inferior frontal cortex [49].
̢̻̉ Resting-state functional MRI
Patients with AD have shown functional disconnection within DMN regions, such as decreased functional connectivity between precuneus and left hippocampus [50]. Recently, cognitively normal elderly with Aβ load have presented the changed functional connectivity between regions within the DMN before the appearance of cognitive decline and behavioral symptoms. Sheline et al. have confirmed that those with brain amyloid deposition have significantly reduced functional connectivity linking precuneus to hippocampus, parahippocampus, anterior cingulate, etc., but increased functional connectivity with visual cortex, which is in line with the changed functional patterns of AD patients [51]. These consequences offer sufficient evidences that Aβ toxicity can be detected early via resting state fMRI. Another study has revealed that Aβ deposition is closely related to the decreased functional connectivity of perihinal cortex in the medial temporal lobe, but has no relationship with cognitive impairment and brain atrophy, indicating that abnormalities of functional connectivity within medial temporal lobe may be the earliest biomarker of preclinical AD before the occurrence of brain structural changes [52]. The mechanism that DMN is specifically targeted by Aβ may be the hyperactivation of DMN regions. The primary components of DMN, including medial prefrontal cortex, posterior cingulate, precuneus, inferior parietal lobe, etc., have higher functional connectivity with other brain regions. These key brain regions, also called hubs, play a crucial role in integrating the global brain information process and their consistent neural activities may intrigue or accelerate the accumulation of Aβ [53-55]. Additionally, functional disconnection within DMN regions are associated with the level of Aβ. Compared with subjects who deposit less Aβ in the brain, cognitively normal adults with more Aβ deposition have significantly decreased functional connectivity [39].
Besides DMN, there are several other brain networks involving sensorimotor and complex cognitive function, such as dorsal attention network (DAN), frontoparietal control network (FPCN), salience network (SN), etc [56]. Changed functional connectivity within these brain networks have been confirmed, indicating that AD-related pathology not only disrupts DMN regions, but attacks other brain networks. Elman et al. found the decreased functional connectivity in the right FPCN and DAN for Aβ-positive asymptomatic elderly, demonstrating that Aβ-related dysfunction involves in multiple brain networks [57]. However, functional connectivity is not limited within a special network. Relatively pivotal brain hub regions have built widespread functional connectivities with other networks for achieving effective information communication. Therefore, patients with AD present disruptions both in with-network local connectivity and between-network global connectivity, which is similar to the altered patterns in the preclinical stage of AD. Drzezga et al. also showed that cognitively normal adults had reduced functional connectivity between posterior cingulated/ precuneus and global brain regions and simultaneously decreased metabolism in those regions, which is consistent with MCI patients with the evidence of Aβ deposition in the brain and further confirmed the relationship between changed functional connectivity and brain hypometabolism [58]. Based on the independent component analysis (ICA), an approach of extracting distributed sets of brain regions with correlated fluctuating activity, Elman et al. found the existence of functional connectivity among multiple brain networks affected by the level of Aβ in the brain [57]. Increased global Aβ contributed to the raised functional connectivity between the anterior PFCN and DMN regions, but decreased relationship between anteriorventral SN and precuneus/DMN. Moreover, Aβ accumulation is also associated with the reduced network efficiency in the cerebrum-cerebellum system [58,59]. Finally, functional activities for preclinical AD are summarized in Table 2. We also clarify the relationship among each neuroimaging modality in Figure 1.
| Study | Techniques | Subjects | Sample | Task/Resting | Main results |
|---|---|---|---|---|---|
| Edelman, et al. [44] | fMRI | CN | 21PIB (+); 23PIB (-) |
Face-name memory-encoding task | Aβ deposition is associated with increased medial temporal lobe activation during memory encoding in preclinical AD. |
| Leal, et al. [45] | fMRI | CN | 45 | Memory task | Increased hippocampal activation is related to subsequent Aβ deposition and cognitive decline. |
| Huijbers, et al. [46] | fMRI | CN | 79 | Episodic memory task | Neocortical Aβ deposition is linked to neuronal dysfunction specifically in entorhinal cortex. |
| Oh & Jagust, [47] | fMRI | CN | 36 elderly; 15 young subjects |
Incidental episodic encoding task | Frontotemporal network connectivity during memory encoding is increased in aging without Aβ deposition in compensating for reduced regional activity, but disrupted by Aβ. |
| Oh, et al., [48] | fMRI | CN | 57 elderly; 42 young subjects |
Working memory (WM) task | Aβ-related hyperactivation is not specific to the episodic memory system but occurs in the frontoparietal control regions as well. |
| Oh, et al, [49] | fMRI | CN | 62 elderly; 43 young subjects |
Executive contextual task | Aβ deposition is associated with decreased right prefrontal activation during task switching. |
| Sheline, et al. [51] | fMRI | CN; AD |
68; 35 |
Resting state | 1. Aβ deposition disrupt resting state default mode network connectivity in preclinical AD; 2. Early manifestation of Aβ toxicity can be detected using resting state fMRI. |
| Song, et al. [52] | fMRI | CN | 56 | Resting state | 1. Aβ load is related to disrupted intrinsic functional connectivity of the perirhinal cortex; 2. Dysfunction in the medial temporal lobe may represent a very early sign of preclinical AD and may predict future memory loss. |
| Hedden, et al. [39] | fMRI | CN | 38 | Resting state | CN with high amyloid burden display significantly reduced functional correlations within the default network relative to CN with low amyloid burden. |
| Elman, et al. [57] | fMRI | CN | 92 | Resting state | 1. Besides DMN, changes of within-network functional connectivity occur in multiple networks; 2. Between-network functional connectivity changes are also apparent. |
| Drzezga, et al. [58] | fMRI; sMRI; FDG-PET |
CN; MCI |
24; 13 |
Resting state | Functional disconnection and hypometabolism display spatially overlap and may represent early functional changes involving Aβ deposition before the onset of AD clinical symptoms. |
| Steininger, et al. [59] | fMRI | CN | 15 | Resting state | Amyloidosis in CN will disrupt brain network efficiency within the cerebro-cerebellar system. |
Table 2: Summary of brain functional changes for preclinical AD based on Fmri.
Future Directions
Recently, almost all of clinical trials involved in drugs targeting Aβ have ended up with failure. Due to the vast loss of neuron and widespread brain atrophy at the stage of dementia, therapeutic intervention focusing on patients with mild or moderate AD are less effective. Therefore, the proposition of term “preclinical AD” has a great potential to markedly prompt series of studies involving the secondary prevention of AD, further providing essential theoretical basis for achieving early diagnosis and preventing the process of AD. The long symptom-free phase of AD is also a crucial stage for fully understanding the brain information integration and the earliest neural alterations before cognitive decline.
At present, AD is regarded as a complex symptom with the interaction between characteristic genetic mutations and environmental changes. Multiple factors, such as age, sex, education, ApoE genotype, etc., would modulate the ultimate clinical profiles of AD [60,61]. In the future, the effects of those established risk factors (e.g. aging, low educational level, obesity) on memory, brain structure and Aβ load are supposed to be considered in preclinical AD studies. Additionally, the combination of various biomarkers derived from multimodal neuroimaging techniques and biochemical methods may contribute to identify high-risk individuals with great possibility of conversion to AD from those without clinical symptoms. Meanwhile, based on big data and machine learning methods, employing patterns of structural and functional information in classification is required to improve the diagnostic precision of AD in the asymptomatic stage.
Acknowledgments
This review was supported by the National Key Research and Development Program of China (2016YFC1306300), National Natural Science Foundation of China (Grant No. 31371007, 81430037, 61633018), Beijing Nature Science Foundation (7161009), Beijing Municipal Science & Technology Commission (Z131100006813022, Z161100002616020), Beijing Municipal government (PXM2017_026283_000002), Fundamental and Clinical Cooperative Research Program of Capital Medical University (16JL-L08).
Financial Disclosures
There are no conflicts of interest for any of the authors related to the work described in the article.
References
- Sperling RA, Aisen PS, Beckett LA, et al. Toward defining the preclinical stages of Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers. Dement 7(1), 280-292 (2011).
- Dubois B, Hampel H, Feldman HH, et al. Preclinical Alzheimer's disease: Definition, natural history, and diagnostic criteria. Alzheimers. Dement 12(1), 292-323 (2016).
- Brys M, Pirraglia E, Rich K, et al. Prediction and longitudinal study of CSF biomarkers in mild cognitive impairment. Neurobiol. Aging 30(1), 682-690 (2009).
- Dubois B, Feldman HH, Jacova C, et al. Advancing research diagnostic criteria for Alzheimer's disease: the IWG-2 criteria. Lancet. Neurol 13(1), 614-629 (2014).
- Sheng C, Huang Y, Han Y. Dissection of prodromal Alzheimer's disease. Front. Biosci (Landmark Ed) 23(1), 1272-1291 (2018).
- Suckling J, Simas T, Chattopadhyay S, et al. A Winding Road: Alzheimer's Disease Increases Circuitous Functional Connectivity Pathways. Front. Comput. Neurosci 9(1), 140 (2015).
- Montembeault M, Rouleau I, Provost JS, et al. Altered Gray Matter Structural Covariance Networks in Early Stages of Alzheimer's Disease. Cereb. Cortex 26(1), 2650-2662 (2016).
- Gomez-Ramirez J, Wu J. Network-based biomarkers in Alzheimer's disease: review and future directions. Front. Aging. Neurosci 6(1), 12 (2014).
- Dubois B, Feldman HH, Jacova C, et al. Research criteria for the diagnosis of Alzheimer's disease: revising the NINCDS-ADRDA criteria. Lancet. Neurol 6(1), 734-746 (2007).
- Dubois B, Feldman HH, Jacova C, et al. Revising the definition of Alzheimer's disease: a new lexicon. Lancet. Neurol 9(1), 1118-1127 (2010).
- Jack CR Jr, Vemuri P, Wiste HJ, et al. Evidence for ordering of Alzheimer disease biomarkers. Arch. Neurol 68(1), 1526-1535 (2011).
- Sheline YI, Raichle ME. Resting state functional connectivity in preclinical Alzheimer's disease. Biol. Psychiatry 74(1), 340-347 (2013).
- Jack CR Jr., Holtzman DM Biomarker modeling of Alzheimer's disease. Neuron 80(1), 1347-1358 (2013).
- Vos SJ, Xiong C, Visser PJ, et al. Preclinical Alzheimer's disease and its outcome: a longitudinal cohort study. Lancet Neurol 12(1), 957-965 (2013).
- Fennema-Notestine C, McEvoy LK, Hagler DJ, Structural neuroimaging in the detection and prognosis of pre-clinical and early AD. Behav. Neurol 21(1), 3-12 (2009).
- Whitwell JL, Przybelski SA, Weigand SD, et al. 3D maps from multiple MRI illustrate changing atrophy patterns as subjects progress from mild cognitive impairment to Alzheimer's disease. Brain 130(1), 1777-1786 (2007).
- Korf ES, Wahlund LO, Visser PJ, et al. Medial temporal lobe atrophy on MRI predicts dementia in patients with mild cognitive impairment. Neurology 63(1), 94-100 (2004).
- Besson FL, La Joie R, Doeuvre L, et al. Cognitive and Brain Profiles Associated with Current Neuroimaging Biomarkers of Preclinical Alzheimer's Disease. J. Neurosci 35(1), 10402-10411 (2015).
- Tondelli M, Wilcock GK, Nichelli P, et al. Structural MRI changes detectable up to ten years before clinical Alzheimer's disease. Neurobiol. Aging 33(1), 825.e825-836 (2012).
- Miller MI, Ratnanather JT, Tward DJ, et al. Network Neurodegeneration in Alzheimer's Disease via MRI Based Shape Diffeomorphometry and High-Field Atlasing. Front. Bioeng. Biotechnol 3(1), 54 (2013).
- Schroeder C, Park MTM, Germann J, et al. Hippocampal shape alterations are associated with regional Abeta load in cognitively normal elderly individuals. Eur. J Neurosci 45(1), 1241-1251 (2017).
- Younes L, Albert M, Miller MI. Inferring changepoint times of medial temporal lobe morphometric change in preclinical Alzheimer's disease. Neuroimage. Clin 5(1), 178-187 (2014).
- Miller MI, Younes L, Ratnanather JT, et al. The diffeomorphometry of temporal lobe structures in preclinical Alzheimer's disease. Neuroimage. Clin 3(1), 352-360 (2015).
- Soldan A, Pettigrew C, Lu Y, et al. Relationship of medial temporal lobe atrophy, APOE genotype, and cognitive reserve in preclinical Alzheimer's disease. Hum. Brain Mapp 36(1), 2826-2841 (2015).
- Mattsson N, Insel PS, Nosheny R, et al. Emerging beta-amyloid pathology and accelerated cortical atrophy. JAMA. Neurol 71(1), 725-734 (2014).
- Fortea J, Vilaplana E, Alcolea D, et al. (2014) Cerebrospinal fluid beta-amyloid and phospho-tau biomarker interactions affecting brain structure in preclinical Alzheimer disease. Ann. Neurol 76(1), 223-230 (2014).
- Pegueroles J, Vilaplana E, Montal V, et al. Longitudinal brain structural changes in preclinical Alzheimer's disease. Alzheimers. Dement 13(1), 499-509 (2017).
- Tijms BM, Kate MT, Wink AM, et al. Gray matter network disruptions and amyloid beta in cognitively normal adults. Neurobiol. Aging 37: 154-160 (2016).
- Brown JA, Terashima KH, Burggren AC, et al. Brain network local interconnectivity loss in aging APOE-4 allele carriers. Proc. Natl. Acad. Sci. U S A 108(1), 20760-20765 (2011).
- Shu N, Wang Z, Qi Z, et al. Multiple diffusion indices reveals white matter degeneration in Alzheimer's disease and mild cognitive impairment: a tract-based spatial statistics study. J. Alzheimers. Dis 26 Suppl 3: 275-285 (2011).
- Zhuang L, Wen W, Zhu W, et al. White matter integrity in mild cognitive impairment: a tract-based spatial statistics study. Neuroimage 53(1), 16-25 (2010).
- Lee SH, Coutu JP, Wilkens P, et al. Tract-based analysis of white matter degeneration in Alzheimer's disease. Neuroscience 301(1), 79-89 (2015).
- Molinuevo JL, Ripolles P, Simo M, et al. White matter changes in preclinical Alzheimer's disease: a magnetic resonance imaging-diffusion tensor imaging study on cognitively normal older people with positive amyloid beta protein 42 levels. Neurobiol. Aging 35(1), 2671-2680 (2014).
- Kantarci K, Schwarz CG, Reid RI, et al. White matter integrity determined with diffusion tensor imaging in older adults without dementia: influence of amyloid load and neurodegeneration. JAMA. Neurol 71(1), 1547-1554 (2014).
- Jacquemont T, De Vico Fallani F, Bertrand A, et al. Amyloidosis and neurodegeneration result in distinct structural connectivity patterns in mild cognitive impairment. Neurobiol. Aging 55(1), 177-189 (2017).
- Pereira JB, van Westen D, Stomrud E, et al. Abnormal Structural Brain Connectome in Individuals with Preclinical Alzheimer's Disease. Cereb. Cortex 1-12 (2017).
- Biswal B, Yetkin FZ, Haughton VM, et al. Functional connectivity in the motor cortex of resting human brain using echo-planar MRI. Magn. Reson. Med 34(1), 537-541 (1995).
- Selkoe DJ. Soluble oligomers of the amyloid beta-protein impair synaptic plasticity and behavior. Behav. Brain. Res 192(1), 106-113 (2008).
- Hedden T, Van Dijk KR, Becker JA, et al. Disruption of functional connectivity in clinically normal older adults harboring amyloid burden. J. Neurosci 29(1), 12686-12694 (2009).
- Han Y, Lui S, Kuang W, et al. Anatomical and functional deficits in patients with amnestic mild cognitive impairment. PLoS. One 7(1), e28664 (2012).
- Sperling RA, Dickerson BC, Pihlajamaki M, et al. Functional alterations in memory networks in early Alzheimer's disease. Neuromolecular. Med 12(1), 27-43 (2010).
- Das SR, Pluta J, Mancuso L, et al. Increased functional connectivity within medial temporal lobe in mild cognitive impairment. Hippocampus 23(1), 1-6 (2013).
- Sheng C, Xia M. Abnormal global functional network connectivity and its relationship to medial temporal atrophy in patients with amnestic mild cognitive impairment. 12(1), e0179823 (2017).
- Edelman K, Tudorascu D, Agudelo C, et al. Amyloid-Beta Deposition is Associated with Increased Medial Temporal Lobe Activation during Memory Encoding in the Cognitively Normal Elderly. Am. J. Geriatr. Psychiatry 25(1), 551-560 (2017).
- Leal SL, Landau SM, Bell RK. Hippocampal activation is associated with longitudinal amyloid accumulation and cognitive decline. Elife 6 (2017).
- Huijbers W, Mormino EC, Wigman SE, et al. Amyloid deposition is linked to aberrant entorhinal activity among cognitively normal older adults. J. Neurosci 34(1), 5200-5210 (2014).
- Oh H, Jagust WJ. Frontotemporal network connectivity during memory encoding is increased with aging and disrupted by beta-amyloid. J. Neurosci 33(1), 18425-18437 (2013).
- Oh H, Steffener J, Razlighi QR, et al. Abeta-related hyperactivation in frontoparietal control regions in cognitively normal elderly. Neurobiol. Aging 36(1), 3247-3254 (2015).
- Oh H, Steffener J, Razlighi QR, et al. beta-Amyloid Deposition Is Associated with Decreased Right Prefrontal Activation during Task Switching among Cognitively Normal Elderly. J. Neurosci 36(1), 1962-1970 (2016).
- Supekar K, Menon V, Rubin D, et al. Network analysis of intrinsic functional brain connectivity in Alzheimer's disease. PLoS. Comput. Biol 4(1), e1000100 (2008).
- Sheline YI, Raichle ME, Snyder AZ, , et al. Amyloid plaques disrupt resting state default mode network connectivity in cognitively normal elderly. Biol. Psychiatry 67(1), 584-587 (2010).
- Song Z, Insel PS, Buckley S, et al. Brain amyloid-beta burden is associated with disruption of intrinsic functional connectivity within the medial temporal lobe in cognitively normal elderly 35(1), 3240-3247 (2015).
- Buckner RL, Sepulcre J, Talukdar T, et al. Cortical hubs revealed by intrinsic functional connectivity: mapping, assessment of stability, and relation to Alzheimer's disease. J. Neurosci 29(1), 1860-1873 (2009).
- Krajcovicova L, Marecek R, Mikl M, et al. Disruption of resting functional connectivity in Alzheimer's patients and at-risk subjects. Curr. Neurol. Neurosci .Rep 14: 491 (2014).
- Simic G, Babic M, Borovecki F, et al. Early failure of the default-mode network and the pathogenesis of Alzheimer's disease. CNS. Neurosci. Ther 20(1), 692-698 (2014).
- Cole MW, Repovs G, Anticevic A. The frontoparietal control system: a central role in mental health. Neuroscientist 20(1), 652-664 (2014).
- Elman JA, Madison CM, Baker SL, et al. Effects of Beta-Amyloid on Resting State Functional Connectivity Within and Between Networks Reflect Known Patterns of Regional Vulnerability. Cereb. Cortex 26(1), 695-707 (2016).
- Drzezga A, Becker JA, Van Dijk KR, et al. Neuronal dysfunction and disconnection of cortical hubs in non-demented subjects with elevated amyloid burden. Brain 134(1), 1635-1646 (2011).
- Steininger SC, Liu X, Gietl A, et al. Cortical Amyloid Beta in Cognitively Normal Elderly Adults is Associated with Decreased Network Efficiency within the Cerebro-Cerebellar System. Front. Aging. Neurosci 6(1), 52 (2014).
- Jack CR Jr, Wiste HJ, Weigand SD, et al. Age, Sex, and APOE epsilon4 Effects on Memory, Brain Structure, and beta-Amyloid Across the Adult Life Span. JAMA. Neurol 72(1), 511-519 (2015).
- Xu W, Yu JT, Tan MS, et al. Cognitive reserve and Alzheimer's disease. Mol. Neurobiol 51(1), 187-208 (2015).