Research Article - Neuropsychiatry (2018) Volume 8, Issue 3
Mortality and Risk Factors in Psychiatric Inpatient with Dementia: A 13-year Long-Term Data Analysis
- Corresponding Author:
- Kuei-Ru Chou
School of Nursing, College of Nursing, Taipei Medical University, Taipei, Taiwan
Tel: 886-2-2736-1661
Fax: 886-2-23772842
Abstract
ABSTRACT
Objective:
The study aimed at identifying mortality and risk factors of psychiatric inpatients with dementia, a 13-year long-term data analysis.
Method:
This study adopted retrospective cohort design. The original claims data of 1 million randomly sampled beneficiaries between 1997 and 2010 from Taiwan’s National Health Insurance Research Database were analyzed. Mortality risk and risk factors were assessed using Cox regression analysis.
Results:
Among 320 dementia patients, a total of 83.4% had Alzheimer disease and 16.6% had vascular dementia. The mortality rates within 1 year after admission were reported for patients with vascular dementia (41.7%) and patients with Alzheimer disease (19.1%). A 1-year increase in age was associated with 3% increase in the risk of hospitalization mortality. Mortality risk among male inpatients was 2.9 times higher than that of female inpatients (P<0.001). The mortality risks among delirium inpatients, those with delusional symptoms, and those with depression had hazard ratios of 2.84 (P=0.004), 2.17 (P=0.008), and 1.82 (P=0.075) respectively, relative to inpatients with uncomplicated symptoms.
Conclusion:
The factors that influenced the mortality of dementia patients admitted to the psychiatric department were male sex, old age, delirium symptoms, and delusional symptoms.
Keywords
Dementia, Mortality risks, Uncomplicated, Delirium, Delusional, Depression
Introduction
Worldwide, approximately 47 million people have dementia, and this number is expected to increase to 131 million by 2050. The worldwide cost of dementia is US$818 billion [1]. According to the demographic statistics released by Taiwan’s Ministry of Interior in September 2017, 243,430 people aged 65 years or older have dementia; they account for 1.09% of the total population in Taiwan, which means that one in every 100 people in Taiwan has dementia [2].
Dementia is generally degenerative and vascularbased in nature. The most common forms of dementia are Alzheimer disease (AD) and vascular dementia (VaD) [3-5]. According to the Diagnostic and Statistical Manual of Mental Disorders (4th Edition Text Revision) (DSM-Ⅳ- TR), dementia is classified by its primary clinical symptoms of accompanying uncomplicated symptoms, delirium, delusions, and depression [4]. Dementia is a combination of symptoms that causes deterioration in memory, language ability, spatial orientation, calculation ability, judgment, abstract thinking ability, and attention. It also leads to behavioral disturbances and personality change, influencing interpersonal relationships and the ability to perform daily living activities [6]. More than 90% of people with dementia develop at least one behavioral or psychological symptom such as sleep problems, paranoia and/or delusions, diurnal disturbance, and aggressiveness during the course of the disease [5,7,8]. Behavioral and psychological symptoms of dementia (BPSD) inflict pain on patients and impose considerable burden on the patients’ caregivers and families as well as the society [9,8]. Severe BPSD requires hospitalization for treatment [10], and the primary reasons patients with dementia are admitted to psychiatric wards include defiant behavior (physically or verbally aggressive behavior), hyperactivity (wandering, restless, or repetitive behavior), or apathy and/or depression (loss of appetite, refusal to eat, refusal to take medication, or suicide) [11,12].
Studies comparing the survival rates of patients with or without dementia have demonstrated increased mortality risks among dementia patients [13-15]. A meta-analysis reported that the mortality of patients with dementia was 15.3% compared to 8.7% of the patients without dementia [16]. The average years of survival from dementia ranges from 1 to 13 years, depending on the age, gender, the type of dementia, and the research design. Therefore, family involvement is one critical aspect that needs to be addressed among dementia people, as it will allow the family members to understand the fatal risk and survival life span of dementia, hence they will be able to make plans as needed [17]. Studies that have investigated the mortality rate and factors of dementia showed that age and gender are possibly related to the mortality rate of dementia and that the mortality rate of dementia increases with age [15,17,18-21]. Other studies have shown that female dementia patients exhibited lower mortality risk than their male counterparts [15,17-24]. Limited studies have compared the different types of dementia and their associated mortality risk, and the results have been inconsistent. Some studies showed that the mortality risk of VAD is higher than AD while other studies showed that the mortality risks of both types are similar. Further, these studies only focused on the community, clinical and outpatient patients [25-28]. Dementia patients who are hospitalized due to psychiatric and behavioural problems have proved to present with severe symptoms than the community, clinical, or outpatient patients. The survival span and the cause of death vary among these patients. However, not much research studies have investigated on this issue. Nonetheless, the research design and the time of follow up may affect the results of dementia mortality risk and survival span. So far, very limited studies have used the long follow-up research design to investigate the various types of dementia, the associated mortality risks and different symptoms among dementia patients following hospitalization in the psychiatric ward. Therefore, this study aims to use 13 years of follow up to investigate different types of dementia along with different symptoms of dementia in the psychiatric ward and its mortality risks and casual factors. This study will report the gender, age, dementia types, accompanying symptoms, mortality risk, and risk factors, along with dementia type, accompanying symptom, the distribution of the time of death and the common disease diagnosis.
Methods
▪ Study design
The National Health Insurance (NHI) was implemented in Taiwan on March 1, 1995. The NHI coverage rate is currently more than 99%, covering almost every citizen in Taiwan. Therefore, the NHI database is a representative database containing empirical data that can be used by medical health care communities. The research outcomes obtained using the database can serve as the basis for medical health care policies. In this study, data were sourced from the Longitudinal Health Insurance Database 2005 (LHID 2005) of the National Health Insurance Research Database (NHIRD). LHID 2005 contains the insurance claims data of one million beneficiaries randomly sampled from the NHIRD in 2005. The NHI report showed no significant difference regarding gender, age, and insured salary in the LHID2005 and NHIRD, suggesting that the data in LHID 2005 can represent the parent population. The LHID2005 contains demographic information, hospital admission records, and treatment procedures undertaken. The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) was adopted in this study. Data were pseudonymized in a pro-con analysis to protect the privacy of these patients and hence informed consent was waived. This retrospective analysis study was approved by the Joint Institutional Review Board of Tri-Service General Hospital (TSGH IRB No.2-106-05- 029).
▪ Study population
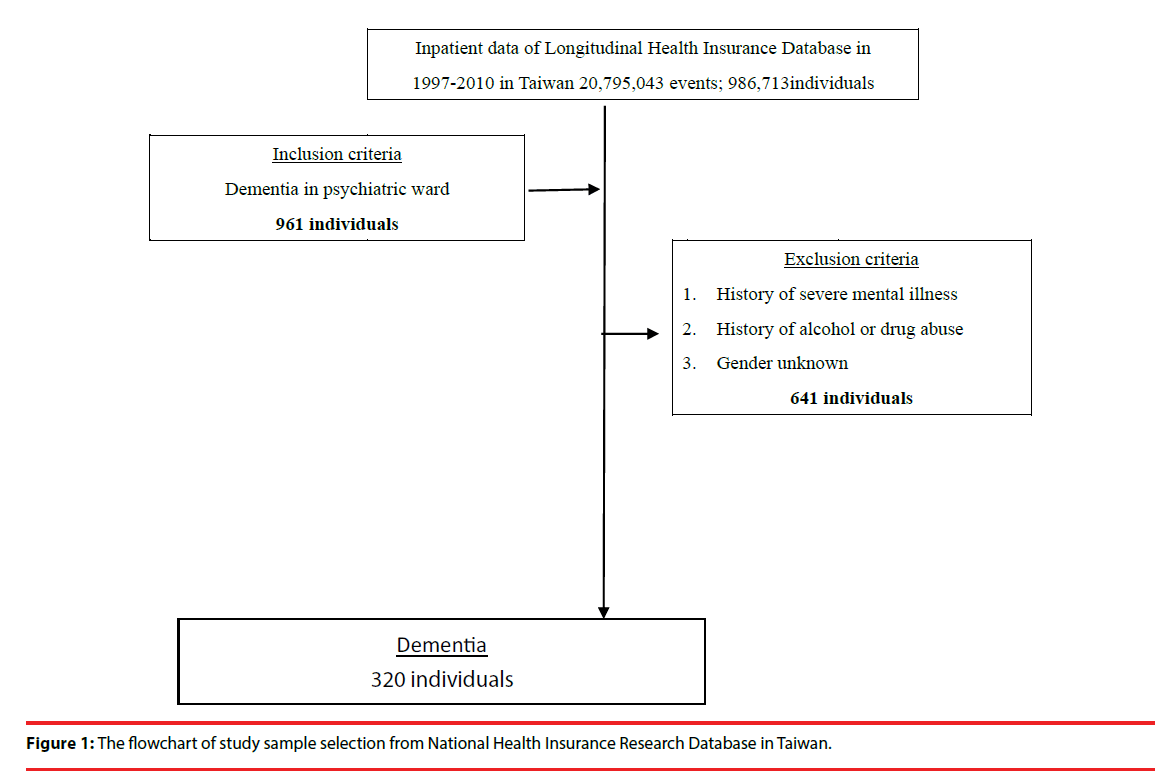
This study obtained one million samples from LHID 2005 (986,713 samples satisfied the inclusion criteria). According to the diagnostic standards in the DSM-IV TR, the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code for dementia is 290 (290.4, 290.0, 290.1, 290.3, 290.20, 290.21). The total number of patients admitted to the psychiatric ward was 961. After patients with a history of severe mental illness, those with a history of alcohol or drug abuse (ICD-9: 291, 292, 293, 294, 295, 296, 304), and those with incomplete data (e.g., gender and age unknown) were excluded, data of 320 patients were incorporated for data analysis (Figure 1).
▪ Statistical analysis
Clinical comorbidity index (CCI) scores were calculated before performing data analysis [29]. In the data analysis, continuous variable results were expressed as means and standard deviations, whereas categorical variables were expressed as numbers and percentages. Chi-square was used to analyze the difference between the categorical variables, and continuous variables were compared using one-way analysis of variance (ANOVA). Mortality risk and risk factors were assessed using Cox regression analysis. All statistical analyses were performed using IBM SPSS Statistics 22.0, with p<0.05 being defined as statistically significant.
Results
▪ Demographic characteristics
Table 1 shows that the 320 patients comprised mostly men (73.8%) and aged between 75 and 84 years (50.0%). Each patient stayed in the hospital for an average of 248.83 days; the average total medical cost amounted to US$19,483.34; and the average number of times of hospitalization was 9.62 (28 patients (9.1%) were hospitalized only once). Inpatient psychiatric admissions were classified into types of dementia (where AD showed the highest prevalence (83.4%)) and accompanying symptoms (where delusions were observed in most of the patients (48.8%), followed by uncomplicated symptoms (22.5%), depression (15.3%), and delirium symptoms (13.4%)). A total of 101 patients (31.6%) died during hospitalization.
| Variables | No. / Mean | % / SD(±) |
|---|---|---|
| Gender | ||
| Male | 236 | 73.8% |
| Female | 84 | 26.3% |
| Type | ||
| VaD | 53 | 16.6% |
| AD | 267 | 83.4% |
| Accompanying symptoms | ||
| uncomplicated | 72 | 22.5% |
| delirium | 43 | 13.4% |
| delusional | 156 | 48.8% |
| depression | 49 | 15.3% |
| Age (years) | ||
| <64 | 21 | 6.6 |
| 65-74 | 56 | 17.5 |
| 75-84 | 160 | 50.0 |
| >85 | 83 | 25.9 |
| Level of care | ||
| Hospital center | 55 | 17.2% |
| Regional hospital | 122 | 38.1% |
| Local hospital | 143 | 44.7% |
| Surgery | ||
| Without | 286 | 89.4% |
| With | 34 | 10.6% |
| Mortality | 101 | 31.6% |
| Charlson Comorbidity Index (CCI) | 1.21 | 1.19 |
| Length of days | 248.83 | 411.88 |
| Medical cost (US$) | 19,483.34 | 24,050.1 |
| Inpatients times | 9.62 | 11.18 |
Table 1: Social demographic characteristics of patients with dementia who are admitted to the psychiatric department (n=320).
Table 2 presents a gender comparison, showing that male and female patients mostly aged 75– 84 years (48.7% vs. 53.6%). Mortality rate for male inpatients was higher than that for female inpatients (26.3% vs. 5.3%, P=.009). The average length of hospital stay for male patients was 2.43 HR longer than that for female patients (294.2 vs. 121.3; P=0.001). The average number of times male patients were hospitalized was also higher than that for female patients (10.9 vs. 6.2; P=0.001). The medical cost of male patients was 1.51 HR higher than that of female patients (US$21,551.6 vs. US$14,290.8; P=0.018). Most male and female patients exhibited AD (72.7% vs. 27.3%) and delusional symptoms (50.4% vs. 44.0%). The research samples were classified by type of dementia into VaD and AD. The number of patients with AD was higher than that of patients with VaD (267 vs. 53). VaD and AD were most prevalent in male patients (79.2% vs. 72.7%). Regarding age distribution, VaD and AD were most prevalent in patients aged 75-84 years (52.8% vs. 49.4%, p<0.001), and VaD and AD were least prevalent in patients aged 85 years or older and 64 years or younger, respectively. In terms of accompanying symptoms, VaD was mostly accompanied by uncomplicated symptoms (34.0%) and was least associated with depression (15.1%). AD was mostly accompanied by delusional symptoms (53.2%) and was least associated with delirium (11.2%). Additionally, VaD and AD demonstrated statistically nonsignificant differences in terms of the patients’ CCI, total average length of hospital stay, total average medical cost, and average number of times of hospitalization (Table 3).
| Variables | Male n= 236 |
Female n= 84 |
p value | ||
|---|---|---|---|---|---|
| No./ Mean | % / SD(±) | No./ Mean | % / SD(±) | ||
| Type | 0.320 | ||||
| VaD | 42 | 79.2% | 11 | 20.8% | |
| AD | 194 | 72.7% | 73 | 27.3% | |
| Accompanying symptoms | 0.184 | ||||
| uncomplicated | 48 | 20.3% | 24 | 28.6% | |
| delirium | 29 | 12.3% | 14 | 16.7% | |
| delusional | 119 | 50.4% | 37 | 44.0% | |
| depression | 40 | 16.9% | 9 | 10.7% | |
| Age (years) | 0.421 | ||||
| <64 | 18 | 7.6% | 3 | 3.6% | |
| 65-74 | 39 | 16.5% | 17 | 20.2% | |
| 75-84 | 115 | 48.7% | 45 | 53.6% | |
| >85 | 64 | 27.1% | 19 | 22.6% | |
| Level of care | |||||
| Hospital center | 38 | 16.1% | 17 | 20.2% | 0.002 |
| Regional hospital | 79 | 33.5% | 43 | 51.2% | |
| Local hospital | 119 | 50.4% | 24 | 28.6% | |
| Surgery | 0.857 | ||||
| Without | 211 | 89.4% | 75 | 89.3% | |
| With | 25 | 10.6% | 9 | 10.7% | |
| Mortality | 84 | 26.3% | 17 | 5.3% | 0.009 |
| Charlson Comorbidity Index (CCI) | 1.2 | ± 1.2 | 1.2 | ± 1.1 | 0.783 |
| Length of days | 294.2 | ± 461.9 | 121.3 | ± 160.4 | 0.001 |
| Medical cost (US$) | 21,551.6 | ± 25,960.8 | 14,290.8 | ± 17,682.3 | 0.018 |
| Inpatients times | 10.9 | ± 12.4 | 6.2 | ± 5.3 | 0.001 |
Table 2: Social demographic characteristics of patients with dementia who are admitted to the psychiatric department (gender).
| Variables | VaD n=53 |
AD n= 267 |
p value | ||
|---|---|---|---|---|---|
| No./ Mean | % / SD(±) | No./ Mean | % / SD(±) | ||
| Gender | 0.320 | ||||
| Male | 42 | 79.2% | 194 | 72.7% | |
| Female | 11 | 20.8% | 73 | 27.3% | |
| Accompanying symptoms | 0.001 | ||||
| uncomplicated | 18 | 34.0% | 54 | 20.2% | |
| delirium | 13 | 24.5% | 30 | 11.2% | |
| delusional | 14 | 26.4% | 142 | 53.2% | |
| depression | 8 | 15.1% | 41 | 15.4% | |
| Age (years) | <0.001 | ||||
| <64 | 10 | 18.9% | 11 | 4.1% | |
| 65-74 | 8 | 15.1% | 48 | 18.0% | |
| 75-84 | 28 | 52.8% | 132 | 49.4% | |
| >85 | 7 | 13.2% | 76 | 28.5% | |
| Level of care | |||||
| Hospital center | 12 | 22.6% | 43 | 16.1% | 0.494 |
| Regional hospital | 18 | 34.0% | 104 | 39% | |
| Local hospital | 23 | 43.4% | 120 | 44.9% | |
| Surgery | 0.857 | ||||
| Without | 47 | 88.7% | 239 | 89.5% | |
| With | 6 | 11.3% | 28 | 10.5% | |
| Mortality | 12 | 3.8% | 89 | 27.8% | .126 |
| Charlson Comorbidity Index (CCI) | 1.2 | ±1.1 | 1.2 | ±1.2 | .906 |
| Length of days | 299.2 | ± 599.1 | 238.8 | ± 364.2 | .482 |
| Medical cost (US$) | 17,840.5 | ± 18,530.7 | 20,003.9 | ± 25,245.8 | .469 |
| Inpatients times | 9.9 | ± 13.5 | 9.6 | ± 10.7 | .854 |
Table 3: Social demographic characteristics of patients with dementia who are admitted to the psychiatric department (type).
▪ Disease characteristics
If cases were classified by their primary clinical symptoms into uncomplicated, delirium, delusional, and depressive symptoms and these symptoms were classified by types of dementia, AD was associated with higher rate of uncomplicated, delirium, delusional, and depressive symptoms compared with VaD. In addition, AD and VaD exhibited statistically significant difference (P=0.001). Regarding inpatient surgery, the percentage of inpatient surgery was highest among patients with depressive symptoms (22.4%) followed by patients with delusional symptoms (10.3%), and statistically significant difference was observed (P=0.020). The average length of hospital stay, medical cost, and number of times of hospitalization were the least for patients with delusional symptoms, and these factors showed statistically significant difference (Table 4).
| Variables | uncomplicated n= 72 |
delirium n= 43 |
delusional n= 156 |
depression n= 49 |
p value | ||||
|---|---|---|---|---|---|---|---|---|---|
| No./ Mean | % / SD(±) | No./ Mean | % / SD(±) | No./ Mean | % / SD(±) | No./ Mean |
% / SD(±) | ||
| Diagnosis | 0.001 | ||||||||
| VaD | 18 | 25.0% | 13 | 30.2% | 14 | 9.0% | 8 | 16.3% | |
| AD | 54 | 75.0% | 30 | 69.8% | 142 | 91.0% | 41 | 83.7% | |
| Gender | 0.184 | ||||||||
| Male | 48 | 66.7% | 29 | 67.4% | 119 | 76.3% | 40 | 81.6% | |
| Female | 24 | 33.3% | 14 | 32.6% | 37 | 23.7% | 9 | 18.4% | |
| Age (years) | 0.080 | ||||||||
| <64 | 8 | 11.1% | 4 | 9.3% | 9 | 5.8% | 0 | 0% | |
| 65-74 | 12 | 16.7% | 5 | 11.6% | 24 | 15.4% | 15 | 30.6% | |
| 75-84 | 38 | 52.8% | 20 | 46.5% | 78 | 50.0% | 24 | 49.0% | |
| >85 | 14 | 19.4% | 14 | 32.6% | 45 | 28.8% | 10 | 20.4% | |
| Level of care | 0.090 | ||||||||
| Hospital center | 15 | 20.8% | 3 | 7.0% | 23 | 14.7% | 14 | 28.6% | |
| Regional hospital | 30 | 41.7% | 19 | 44.2% | 60 | 38.5% | 13 | 26.5% | |
| Local hospital | 27 | 37.5% | 21 | 48.8% | 73 | 46.8% | 22 | 44.9% | |
| Surgery | 0.020 | ||||||||
| Without | 67 | 93.1% | 41 | 95.3% | 140 | 89.7% | 38 | 77.6% | |
| With | 5 | 6.9% | 2 | 4.7% | 16 | 10.3% | 11 | 22.4% | |
| Mortality | 21 | 6.6% | 17 | 5.3% | 43 | 13.4% | 20 | 6.3% | 0.208 |
| Charlson Comorbidity Index (CCI) | 1.19 | ± 1.12 | 1.23 | ± 0.95 | 1.28 | ± 1.31 | 1.00 | ± 1.06 | 0.568 |
| Length of days | 353.6 | ± 607.2 | 209.1 | ± 269.5 | 186.4 | ± 261.7 | 328.6 | ± 510.3 | 0.014 |
| Medical cost (US$) | 24,102.4 | ± 27,824.7 | 18,546.5 | ± 20,207.7 | 16,257.1 | ± 20.739.6 | 24,852.8 | ± 30,347.3 | 0.049 |
| Inpatients times | 11.7 | ± 14.1 | 9.8 | ± 12.3 | 7.8 | ± 7.5 | 12.3 | ± 14.1 | 0.024 |
Table 4: Social demographic characteristics of patients with dementia who are admitted to the psychiatric department (accompanying symptoms).
An analysis of 13-year follow-up data revealed that among patients with dementia admitted to the psychiatric department, these patients were hospitalized not only for BPSD treatment, but also for treatment of various diseases. The results indicated that the top five diseases leading to inpatient admissions were pneumonia (n=180/9.0%), urinary tract infection (n=127/6.4%), obstructive chronic bronchitis with acute exacerbation (n=81/4.1%), acute respiratory failure (n=64/3.2%), and unspecified septicemia (n=45/2.3%).
▪ Inpatient mortality diagnosis and distribution of time of death
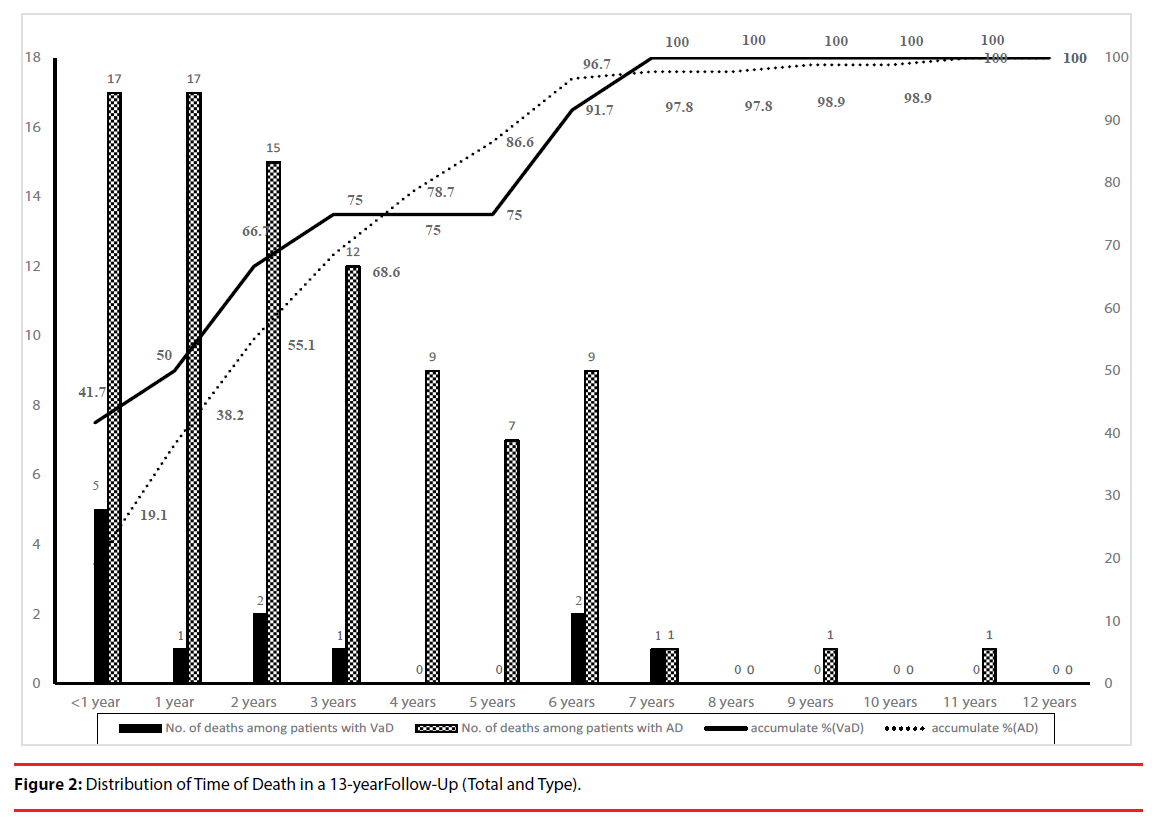
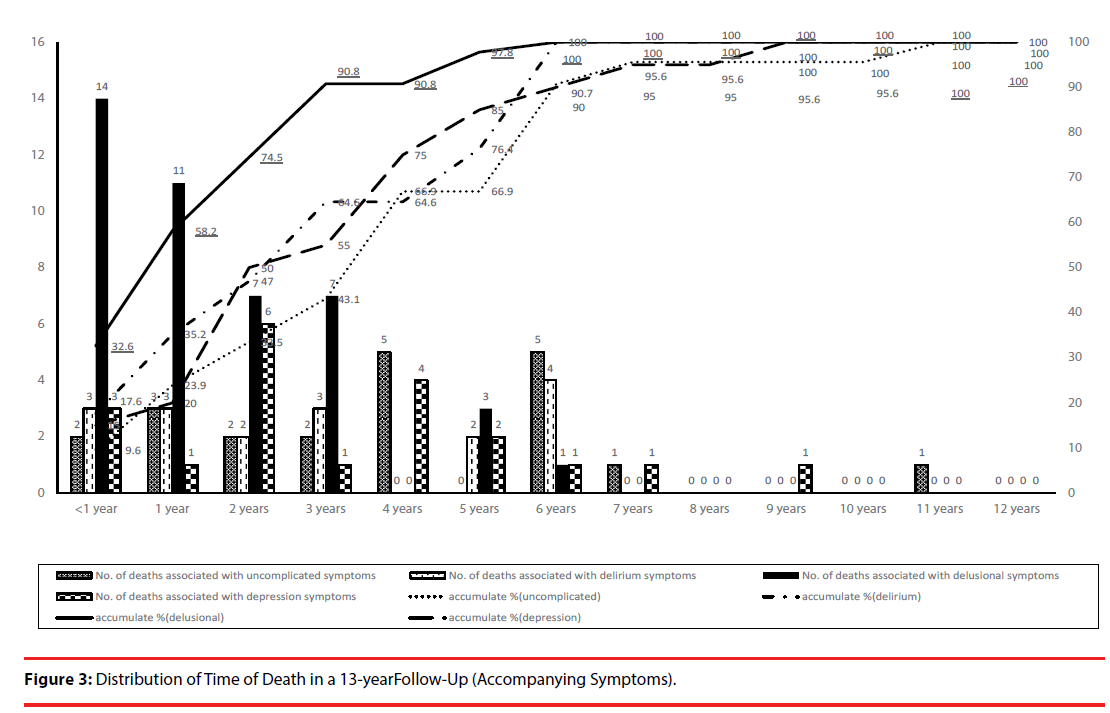
According to a 13-year follow up of patients with dementia who were admitted to the psychiatric department, the top three diseases leading to inpatient mortality were pneumonia (n=32/31.7%), respiratory failure (n=25/24.8%), and septicemia (n=12/11.9%). That in a 13-year follow-up, 101 patients with dementia died during psychiatric admission. More than half of these mortality cases (55.4%) occurred within 2 years, and 96% of the patients died within 6 years. The time of death showed statistically significant differences (P=0.012). In terms of VaD and AD, the distribution of time of death also differed. Noticeably, the time of death for patients with VaD concentrated in the first three years, whereas that for patients with AD was uniformly distributed and showed no substantial difference every year. However, the time of death for patients with AD differed considerably after the sixth year, decreasing from 10.1% to 1.1% in the seventh year (Figure 2). An analysis of time of death based on the four types of symptoms showed that the mortality rate one year after admission to the psychiatric ward was the highest among dementia patients with delusional symptoms (32.6%), followed by those with delirium symptoms (17.6%). In particular, the six-year mortality rate among dementia patients with delirium symptoms and those with delusional symptoms was 100%. These results indicate that the four types of accompanying symptoms differed in terms of time of death, and that the differences were statistically significant (P=0.031) (Figure 3).
▪ Inpatient mortality risk and influencing factors
This study used Cox regression to analyze the mortality risks and risk factors associated with patients with dementia who are admitted to psychiatric department for treatment. After the type of dementia, season, place of residence, level of care, surgery history, and CCI scores were controlled for, the results indicated that the risk factors for psychiatric admission mortality were age, gender, accompanying symptoms, and level of care. Oneyear increase in age is associated with 3% increase in risk of hospitalization mortality. Mortality risk for male inpatients was 2.9 times higher than that for female inpatients (P<0.001). The mortality risks among inpatients with delirium and those with delusional symptoms were 2.84 HR (P=0.004) and 2.17 HR (P=0.008) higher than those among inpatients with uncomplicated symptoms (Table 5), respectively.
| Variables | Adjusted HR | 95% CI | 95% CI | P value |
|---|---|---|---|---|
| Gender | <0.001 | |||
| Male | 2.90 | 1.67 | 5.13 | |
| Female | Reference | |||
| Type | ||||
| AD | 1.32 | 0.72 | 2.40 | 0.358 |
| VaD | Reference | |||
| Accompanying symptoms | ||||
| delirium | 2.84 | 1.40 | 5.75 | 0.004 |
| delusional | 2.17 | 1.23 | 3.83 | 0.008 |
| depression | 1.82 | 0.94 | 3.52 | 0.075 |
| uncomplicated | Reference | |||
| Season | ||||
| Summer (June-August) | 1.32 | 0.73 | 2.39 | 0.355 |
| Autumn (September-November) | 1.33 | 0.72 | 2.46 | 0.365 |
| Winter (December-Feburary) | 0.73 | 0.41 | 1.31 | 0.291 |
| Spring (March-May) | Reference | |||
| Low-income | 0.147 | |||
| With | 0.42 | 0.13 | 1.36 | |
| Without | Reference | |||
| Level of care | ||||
| Hospital center | 0.740 | 0.45 | 1.23 | 0.244 |
| Regional hospital | 0.458 | 0.22 | 0.95 | 0.037 |
| Local hospital | Reference | |||
| Surgery | 0.463 | |||
| With | 1.27 | 0.67 | 2.43 | |
| Without | Reference | |||
| Age (years) | 1.03 | 1.01 | 1.06 | 0.007 |
| Charlson Comorbidity Index (CCI) | 0.99 | 0.84 | 1.16 | 0.882 |
| Length of days | 1.00 | 1.00 | 1.00 | 0.696 |
| Medical cost (US$) | 1.00 | 1.00 | 1.00 | 0.072 |
| Inpatients times | 1.00 | 0.99 | 1.01 | 0.943 |
Table 5: Cox regression model.
Discussion
The results of this study showed that the number of male patients with dementia who were admitted to psychiatric ward was 2.8 HR higher than that of female patients (73.8% vs. 26.3%). In addition, medical cost, length of hospital stay, and number of times of hospitalization were higher among male patients compared with those of female patients. These results differ from previous findings, which showed that the number of female inpatients with dementia was higher than that of male inpatients [8,11,12], but are similar to the result of a previous study (ie, the number of male inpatients was higher than that of female inpatients) [30]. Extant clinical observations and literature showed that male patients with dementia were typically associated with aggressive behavior, regressive behavior, inappropriate behavior, aggression, wandering behavior, and delusions. By contrast, female patients with dementia often exhibit depressive symptoms (eg, crying, sadness, anxiety, and fear), verbal complaints, and hallucinations [31,32]. Numerous past studies have indicated that caregivers of patients with dementia reported disruptive behavior (e.g., aggressive behavior, screaming, physical assaults, and verbal abuse) to be the most difficult, stressful, and helpless situation when caring for these patients. These aggressive behavior or problematic behavior was also the reason prompting caregivers to admit these patients to psychiatric ward for treatment [11,33,34]. This phenomenon possibly explains the higher percentage of male inpatients in the present study.
Previous studies have shown that onset of AD typically occurs after the age of 65 years, and the prevalence of this disease increases with age. In addition, 7% of patients with AD were aged 65–74 years, and 53% of patients with AD were aged 75–84 years [35,36]. In the present study, the rate of BPSD among patients with AD who were admitted to psychiatric department was higher than that among patients with VaD, irrespective of average age or age group. This result is possibly attributed to the earlier onset of patients with VaD compared with patients with AD [35].
Multiple studies have reported that BPSDs among patients with VaD were mostly depressive symptoms, followed by change in dietary behavior, sleep disorder, agitation or aggressive behavior, and delusional symptoms [3,5,37-40]. However, we found that VaD is most commonly associated with uncomplicated symptoms, followed by delusional subtype. This discrepancy is probably caused by the difference in research samples and location. Previous studies generally recruit community residents [38] and patients who visit clinics [3] and hospital inpatient departments [5,39]. Our study samples were inpatients whose symptoms and disease severity differed from those of community-based patients. Moreover, AD in our study was mostly associated with delusional symptoms (53.2%). This result is similar to previous foreign and domestic studies, which reported that the percentage of delusional symptoms was the highest among patients with AD (30–75.2%) [5,38,41].
Inconsistent results have been reported on the mortality risk among patients with VaD and AD. Most of these results revealed that mortality risk among patients with VaD was higher than that among patients with AD; the research participants involved were patients living in a community and those who visited medical clinics, and the follow-up period was 2.5–5 years [17,25,26]. In addition, several studies found that the mortality risks among VaD and patients with AD were similar, and that mortality risk was not related to dementia diagnosis but was related to disease severity. The research participants involved in these studies were inpatients, community residents, and those who visited medical clinics, and the follow-up period was 6–13 years [27,28]. The 13-year follow-up and observation conducted in our study showed that the cumulative mortality risk among patients with VaD and those with AD did not differ considerably; however, the time of death varied substantially between them. For patients with VaD, the mortality rate one year and three years after admission to the psychiatric ward was 41.7% and 75%, respectively. For patients with AD, the mortality rate one year and three years after admission to the psychiatric ward was 19.1% and 68.6%, respectively. Therefore, the discrepancy between the results of past studies comparing the mortality risk of patients with AD and those with VaD is likely related to the different follow-up periods and research participants.
This study determined that in addition to BPSDs, diagnoses most often leading to inpatient psychiatric treatment among patients with dementia were pneumonia and urinary tract infection. This result accords with the findings of previous studies regarding the most common reasons for admission treatment [16,42-44]. In addition, pneumonia was the foremost cause of death in our study, which is similar to the primary cause of deaths reported in previous studies [7,16,45-47]. Several studies have listed multiple factors associated with pneumoniacaused death, and these include infection and dysphagia [45,46]. Use of antipsychotic and benzodiazepine is also a risk factor of pneumonia and mortality [48,49]. Therefore, the risk of pneumonia-caused death is likely to increase after patients with dementia are admitted to psychiatric ward for treatment. Prevention of pneumonia in patients with dementia who are admitted to the psychiatric department is a crucial topic for health care professionals. For patients taking antipsychotic and benzodiazepine treatments, health professionals should adopt measures for infection prevention, encourage patients to receive pneumonia and flu vaccine, and observe conditions of dysphagia in these patients, thereby preventing and reducing the incidence of infection and lowering mortality risk.
Mortality risks and factors associated with psychiatric admission of patients with dementia were male, old age, delirium symptoms, and delusional symptoms. Regarding hospitalization mortality risk, mortality risk for male inpatients was 2.9 HR higher than that for female inpatients. Previous studies have indicated that the mortality rate and mortality risk of male patients with VaD and those with AD were higher than those of female patients irrespective of the place of origin of these patients (ie, community, clinics, or inpatient departments) [17,26,28,50]. This result is similar to the results of the present study regarding patients with dementia admitted to psychiatric wards. We determined that accompanying symptoms were a predictor of hospitalization mortality risk, and that the mortality risks associated with delirium and delusional symptoms were respectively 2.84 HR and 2.17 HR higher than those associated with uncomplicated symptoms. Furthermore, the mortality rate one year after admission to the psychiatric ward was the highest among dementia patients with delusional symptoms followed by those with delirium symptoms. Older age follows higher mortality risk. One-year increase in age is associated with 3% increase in risk of hospitalization mortality, implying that age is also a predictor of hospitalization mortality risk. Multiple studies have reported that the mortality risk of patients with dementia increases with age, particularly patients with VaD and those with AD, whose mortality risk rises as their disability increases in severity with age [8,17,25,26,28,51].
Limitations
The research limitations of this study were as follows. This study involved an analysis of NHIRD, and variables such as education level and marital status were not included in the investigation. This study adopted cross-sectional design, which allows for only an analysis of the association between different variables and not the causal relationships between them. The collected data was based on the hospitalized patients only; and therefore, no data of the patients who died elsewhere was available or analyzed.
Conclusion
The factors that influence the mortality of patients with dementia admitted to psychiatric department were male, old age, delirium symptoms, and delusional symptoms. The mortality rate of patients with VaD one year after admission to the psychiatric ward was higher than that of patients with AD. The 13-year longterm follow-up showed that pneumonia is the most common disease leading to mortality.
For patients with dementia who are admitted to psychiatric department, particularly those with VaD, those with delusional symptoms, those with delirium symptoms, and families of these patients, efforts should be made to prevent respiratory infection, reduce hospitalization mortality rate, and provide BPSD treatments and relevant health education. Future studies could investigate the risks and factors associated with antipsychotic- and pneumonia-caused deaths among patients with dementia who are admitted to a psychiatric department.
Ethical Approval
Joint Institutional Review Board of Tri-Service General Hospital (TSGH IRB No.2-106-05-029).
Conflict of Interest
The authors declare that they have no competing interests.
References
- International AsD (2016) World Alzheimer Report 2016. Improving healthcare for people living with dementia coverage, Quality and costs now and in the future.
- Assoction TAD (2017) Dementia.
- Thompson C, Brodaty H, Trollor J, et al.Behavioral and psychological symptoms associated with dementia subtype and severity. Int. Psychogeriatr 22(2), 300-305 (2010).
- Association AP, Association AP Task Force on DSM-IV. Diagnostic and statistical manual of mental disorders, DSM-IV-TR. Washington, DC, American Psychiatric Association. 4(1) (2000).
- Pinidbunjerdkool A, Saengwanitch S, Sithinamsuwan P. Behavioral and psychological symptoms of dementia. J. Med. Assoc. Thai 97(2), 168-174 (2014).
- Cerejeira J, Lagarto L, Mukaetova-Ladinska EB. Behavioral and psychological symptoms of dementia. Front. Neurol 3(1), (2012).
- Ballard C, Corbett A, Chitramohan R, et al.Management of agitation and aggression associated with Alzheimer's disease, controversies and possible solutions. Curr. Opin. Psychiatry 22(6), 532-540 (2009).
- Lövheim H, Sandman PO, Karlsson S, et al.Behavioral and psychological symptoms of dementia in relation to level of cognitive impairment. Int. Psychogeriatr 20(4), 777-789 (2008).
- Millán-Calenti JC, Lorenzo-López L, Alonso-Búa B, et al.Optimal nonpharmacological management of agitation in Alzheimer’s disease, challenges and solutions. Clin. Interv. Aging 11(1), 175 (2016).
- Sugiyama H, Kazui H, Shigenobu K, et al.Predictors of prolonged hospital stay for the treatment of severe neuropsychiatric symptoms in patients with dementia, a cohort study in multiple hospitals. Int. Psychogeriatr 25(8), 1365-1373 (2013).
- Tochimoto S, Kitamura M, Hino S, et al.Predictors of home discharge among patients hospitalized for behavioural and psychological symptoms of dementia. Psychogeriatrics 15 (4), 248-254 (2015).
- Takacs R, Ungvari GS, Gazdag G Reasons for acute psychiatric admission of patients with dementia. Neuropsychopharmacol. Hung 17(3), 141-145 (2015).
- Tschanz J, Corcoran C, Skoog I, et al.Dementia, The leading predictor of death in a defined elderly population The Cache County Study. Neurology 62(7), 1156-1162 (2004).
- Baldereschi M, Di Carlo A, Maggi S, et al.Dementia is a major predictor of death among the Italian elderly. Neurology 52(4), 709-709 (1999).
- Wolfson C, Wolfson DB, Asgharian M, et al. A reevaluation of the duration of survival after the onset of dementia. N. Engl. J. Med 344(15), 1111-1116 (2001).
- Rao A, Suliman A, Vuik S, et al. Outcomes of dementia: systematic review and meta-analysis of hospital administrative database studies. Arch. Gerontol. Geriat. 66(1), 198-204 (2016).
- Garcia-Ptacek S, Farahmand B, Kareholt I, et al. Mortality risk after dementia diagnosis by dementia type and underlying factors: a cohort of 15,209 patients based on the Swedish Dementia Registry. J. Alzheimers. Dis 41(2), 467-477 (2014).
- Ganguli M, Dodge HH, Shen C, et al. Alzheimer disease and mortality: a 15-year epidemiological study. Arch. Neur 62(5), 779-784 (2005).
- Aguero-Torres H, Fratiglioni L, Guo Z, et al. Mortality from dementia in advanced age: a 5-year follow-up study of incident dementia cases. J. Clin. Epidemiol 52(8), 737-743 (1999).
- Brookmeyer R, Corrada MM, Curriero FC, et al. Survival following a diagnosis of Alzheimer disease. Arch. Neur 59(11), 1764-1767 (2002).
- Xie J, Brayne C, Matthews FE. Survival times in people with dementia: analysis from population based cohort study with 14 year follow-up. Bmj 336 (7638), 258-262 (2008).
- Soto ME, Andrieu S, Villars H, et al. Improving care of older adults with dementia: description of 6299 hospitalizations over 11 years in a special acute care unit. J. Am. Med. Direct. Assoc 13(5), 486.e481-486 (2012).
- Knopman DS, Rocca WA, Cha RH, et al. Survival study of vascular dementia in Rochester, Minnesota. Arch. Neur 60(1), 85-90 (2003).
- Rountree SD, Chan W, Pavlik VN, et al. Factors that influence survival in a probable Alzheimer disease cohort. Alz. Res. Ther 4(3), 16 (2012).
- Michel JP, Pautex S, Zekry D, et al. End-of-life care of persons with dementia. J. Gerontol. Series. Biol. Sci. Med. Sci 57(10), M640-M644 (2002).
- Garcia‐Ptacek S, Kåreholt I, Cermakova P, et al. Causes of Death According to Death Certificates in Individuals with Dementia: A Cohort from the Swedish Dementia Registry. J. Am. Geriat. Soc 64 (11) (2016).
- Bruandet A, Richard F, Bombois S, et al. Alzheimer disease with cerebrovascular disease and vascular dementia, clinical features and course compared with Alzheimer disease. J. Neurol. Neurosurg. Psychiat 80(2), 133-139 (2009).
- Villarejo A, Benito-León J, Trincado R, et al. Dementia-associated mortality at thirteen years in the NEDICES Cohort Study. J. Alzheimer's. Dis 26(3), 543-551 (2011).
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies, Development and validation. J. Chron. Dis 40(5), 373-383 (1987).
- Chang CC, Lin PH, Chang YT, et al. The Impact of Admission Diagnosis on Recurrent or Frequent Hospitalizations in 3 Dementia Subtypes, A Hospital-Based Cohort in Taiwan with 4 Years Longitudinal Follow-Ups. Med 94(46), (2015).
- Lövheim H, Sandman PO, Karlsson S, et al. Sex differences in the prevalence of behavioral and psychological symptoms of dementia. Int. Psychogeriat 21(3), 469-475 (2009).
- Xing Y, Wei C, Chu C, et al. Stage-specific gender differences in cognitive and neuropsychiatric manifestations of vascular dementia. Am. J Alzheimer's. Dis. Dement 27(6), 433-438 (2012).
- Gupta M, Dasgupta A, Khwaja GA, et al. Behavioural and psychological symptoms in poststroke vascular cognitive impairment. Behav. Neurol (2014).
- Miyamoto Y, Tachimori H, Ito H. Formal caregiver burden in dementia, impact of behavioral and psychological symptoms of dementia and activities of daily living. Geriat. Nurs 31(4), 246-253 (2010).
- Spitzer RL, Gibbon ME, Skodol AE, et al. DSM-IV-TR casebook, A learning companion to the diagnostic and statistical manual of mental disorders, text rev. Am. Psychiat. Publish. Inc (2002).
- Association AP. Diagnostic and statistical manual of mental disorders (DSM-5®). Am. Psychiat. Pub (2013).
- D’Onofrio G, Sancarlo D, Panza F, et al. Neuropsychiatric symptoms and functional status in Alzheimer’s disease and vascular dementia patients. Curr. Alzheimer. Res 9(6), 759-771 (2012).
- Lyketsos CG, Steinberg M, Tschanz JT, et al. Mental and behavioral disturbances in dementia, findings from the Cache County Study on Memory in Aging. Am. J. Psychiat 157 (5), 708-714 (2000).
- Fuh J, Wang S, Cummings J. Neuropsychiatric profiles in patients with Alzheimer’s disease and vascular dementia. J. Neurol. Neurosurg. Psychiat 76 (10), 1337-1341 (2005).
- Ballard C, Neill D, O’brien J, et al. Anxiety, depression and psychosis in vascular dementia, prevalence and associations. J. Affect. Disord 59(2), 97-106 (2000).
- Fuh J, Liu C. Study of behavioral and psychological symptoms of dementia in Taiwan. Acta. Neurol. Taiwanica 15(3), 154 (2006).
- Guijarro R, San Román CM, Gómez-Huelgas R, et al. Impact of dementia on hospitalization. Neuroepidemiol 35 (2), 101-108 (2010).
- Bail K, Berry H, Grealish L, et al. Potentially preventable complications of urinary tract infections, pressure areas, pneumonia, and delirium in hospitalised dementia patients, retrospective cohort study. BMJ open 3 (6), e002770 (2013).
- Zhao Y, Kuo TC, Weir S, et al. Healthcare costs and utilization for Medicare beneficiaries with Alzheimer's. BMC. Health. Services. Res 8(1), 108 (2008).
- Manabe T, Mizukami K, Akatsu H, et al. Factors Associated with Pneumonia-caused Death in Older Adults with Autopsy-confirmed Dementia. Int. Med. 56 (8), 907-914 (2017).
- Mitchell SL, Teno JM, Kiely DK, et al. The clinical course of advanced dementia. England. J. Med 361 (16), 1529-1538 (2009).
- Naumova EN, Parisi SM, Castronovo D, et al. Pneumonia and influenza hospitalizations in elderly people with dementia. J. Am. Geriat. Soc 57 (12), 2192-2199 (2009).
- Tolppanen AM, Koponen M, Tanskanen A, et al. Antipsychotic Use and Risk of Hospitalization or Death Due to Pneumonia in Persons With and Those Without Alzheimer Disease. CHEST. J 150(6), 1233-1241 (2016).
- Taipale H, Tolppanen AM, Koponen M, et al. Risk of pneumonia associated with incident benzodiazepine use among community-dwelling adults with Alzheimer disease. CMAJ, Canadian Medical Association journal. J. Canadian. Med. Assoc 189(14), E519-e529 (2017).
- Hinterberger M, Fischer P, Huber K, et al. Leukocyte telomere length is linked to vascular risk factors not to Alzheimer’s disease in the VITA study. J. Neural. Trans 1-11 (2017).
- Brännström J, Boström G, Rosendahl E, et al. Psychotropic drug use and mortality in old people with dementia, investigating sex differences. BMC. Pharmacol. Toxicol 18 (1),36 (2017).