Research Article - Neuropsychiatry (2016) Volume 6, Issue 4
Differentiating bipolar type I and II depression from unipolar depression: the role of clinical features, current symptoms and a past hypomanic symptoms checklist
- Corresponding Authors:
- Guiyun Xu, MD
Department of Affective Disorders
the Affiliated Brain Hospital of Guangzhou Medical University
36 Mingxin Road, LiwanDistrict
Guangzhou, Guangdong Province 510370, China
Telephone: +86 18922165291
Fax: +86 020 81891391
- Kangguang Lin, MD
Laboratory of Emotion and Cognition
the Affiliated Brain Hospital of Guangzhou Medical University
Guangzhou, China
Telephone: +86 020-81268189
Abstract
Background: To explore the role of clinical features, current symptoms and a past hypomanic symptom checklist in distinguishing bipolar from unipolar depression among patients with current major depressive episodes.
Method: Patients with bipolar I disorder (BDI, N=122), bipolar II disorder (BDII, N=160) as well as major depressive disorder (MDD, N=353) were enrolled. We collected clinical features and current symptoms on these patients, asked them to complete a 15-item checklist about prior symptoms of hypomania (HCL-15), and administered the Hamilton Depression Rating Scale.
Results: Multivariate analyses showed that patients with BDI, compared with MDD, were less likely to be female and to endorse the symptoms of diminished interest; more likely to be obesity/overweight and to have more total episodes. Patients with BDII, compared with MDD again, were more likely to have an earlier age onset, more total episodes, more seasonal depressive onset, and to manifest irritable symptoms. Inclusion of HCL-15 in the comparison significantly increased the area under curve of BDII versus MDD.
Conclusion: Our study suggests that clinical features and current symptoms could provide good ability in differentiating BDI from MDD. Combination of clinical features and the result of HCL-15may assist clinicians better to identify BDII.
Trial registration number: This trial was registered in the Chinese Clinical Trial Registry (www. chictr. org) and was assigned ChiCTR-TNRC-10001112 on December 23, 2010.
Keywords
Major depressive episode, Misdiagnosis, Hypomanic checklist, Chinese, SCID-I/P
Introduction
Major depressive episodes (MDE) are prominent in both bipolar disorders (BD) and major depressive disorder (MDD). It is reported that up to 69% of patients with BD have ever been misdiagnosed, and most of them were wrongly diagnosed as MDD [1,2]. Misdiagnosis of BD as MDD often leads to inappropriate treatment strategy [3], and therefore results in poorer prognosis and heavier burden of disease [4,5]. To improve the identification of BD, in the past decades, a number of studies, including western and Chinese samples, have attempted to search for differentiating features from clinical phenomenology, screening instruments or biomarkers [6-9]. The following features were usually found related to BD: early age of onset, family history of BD, atypical features, mixed symptoms, etc. [6,10-15]. Moreover, some screening tools, such as mood disorder questionnaire (MDQ) [16], hypomanic checklist 32(HCL-32) [17,18], and hypomanic checklist 15(HCL-15) [19], were reported to have the potential ability to discriminate BD from MDD. MDQ seems to be sensitive to identify insightful patients with BDI but probably less useful to identify patients with milder form of bipolar disorder, such as BDII [16]. HCL-32 is believed to be a valid questionnaire for the correct identification of both BDI and BDII in clinical and non-clinical settings [17,20]. However, some researchers argue that the length of the HCL-32 may make it less feasible in busy clinical setting. In this circumstance, HCL-15, a short version of HCL-32, was developed to differentiate BD or bipolar spectrum disorder from MDD [21], and fair ability of Chinese version of HCL-15 was found to distinguish BD from MDD in our preliminary study [19]. More recently, some researchers have tried to detect the biological differences between BD and MDD, and most of them focused on the neuroimaging and blood based biomarkers [9,22], which are obtained through expensive equipment or reagents. However, those findings are preliminary and currently not robust or convenient enough to aid in distinguishing BD from MDD, especially for low or middle income countries. Hence, clinical markers, such as life time clinical features, current symptoms, and screening checklist, still play an important role in differentiating BD from MDD.
Previous studies have found that clinical features and current symptomology could provide good ability to discriminate BDI from MDD in the context of MDE, whereas the ability of them to discriminate BDII from MDD was comparatively low [23]. Besides, most of the studies have included too many variables [6,12], and the odd ratios of variables are thus comparatively low, which may affect their feasibility in busy clinical practice [14]. As many past hypomanic symptoms screening tools were proved to be effective in detecting BD, combining a screening tool and clinical features may help us better to distinguish BD from MDD, and thus very likely with lesser variables. Nevertheless, few studies have attempted to simultaneously probe the role of past hypomanic symptoms screening tools, clinical features and current symptoms.
Given these considerations, we compared bipolar depression (BDI+BDII) with unipolar depression in a Chinese population, with an inclusion of appropriate amount of variables covering clinical features, current symptoms as well as past hypo/ manic symptoms evaluated by HCL-15. The goal of the present study was to explore to what extent using clinical features and current symptomatology would help us distinguishing BDI and BDII from MDD in a Chinese clinical sample, and to see whether adding a past hypo/ manic symptoms checklist would help us better in making a correct diagnosis.
Methods
▪ Subjects
The present data derived from the Clinical and Biological Characteristics and Optimizing treatment in Bipolar Disorder projects (June 2007 to November 2010),which was a prospective semi-naturalistic trial aimed to improve the detection of BD in the context of major depressive episode in terms of clinical features and biological markers of BD. The study was conducted in the Guangzhou Brian Hospital and the First Affiliated Hospital of Jinan University. The Guangzhou Brian Hospital is one of the biggest psychiatric hospitals in China. The First Affiliated Hospital of Jinan University is a large comprehensive hospital, which provides both inpatient and outpatient psychiatric service in Guangzhou. Greater detail of the project can be found elsewhere [24].
Consecutive patients who satisfied the inclusion and exclusion criteria were evaluated. The inclusion criteria comprised patients diagnosed with BDI, BDII or MDD; suffering from MDE; aged 18 or above. The exclusion criteria included: currently in manic/hypomanic episode; pregnant or breastfeeding women; clinical and/or laboratory evidence of serious physical conditions; history of seizure disorder or mental retardation; had received electroconvulsive therapy during the previous four weeks.
In phase I, patients suffering from MDE and receiving outpatient or inpatient psychiatric services were referred to the project by their respective first contact psychiatrist. A senior psychiatrist (who had been practicing for more than 10 years) then conducted the Chinese version of Structured Clinical interview for DSM-IV-TR Axis I Disorders patient edition (SCID-I/P) interview. A diagnosis was made, according to the DSM-IV, on the basis of a combination of a consensus of clinical impression, the SCIDI/P interview and a review of medical records. In phase II, Another senior psychiatrist conducted an independent assessment of HCL-15 and Hamilton depression rating scale-17 (HAMD-17) subsequently. The inter-rater reliability for the diagnoses was high (kappa value>0.9). The project was approved by the Ethics Committee of Guangzhou Brain Hospital and administrated at China clinical trial (ChiCTR-TNRC-10001112, http://www.chictr.org). All of the participants gave written informed consent. The present study consisted of 122 patients with BDI, 160 patients with BDII and 353 patients with MDD.
▪ Assessments
Sociodemographic data were obtained through a self-designed questionnaire. The Chinese version of SCID-I/P [2] was used to confirm the diagnosis and obtain some clinical features and current symptoms. Variables about clinical features included age of first onset, number of total episodes, number of hospitalization, precipitating factors before onset, family history about BD, seasonal depressive onset, psychotic feature, catatonic feature, melancholic feature, atypical feature, mixed depression, obesity/ overweight and comorbidity of any anxiety disorders. Mixed depression was defined by current MDE plus 3 or more intra-MDE hypomanic symptoms that lasted at least one week at the time of the interview [11]. Obesity/ overweight was defined by the body mass index that greater than 24according to the criteria for Chinese population [25]. Anxiety disorders included generalized anxiety disorder; panic disorder; social phobia disorder; agoraphobia; special phobia; hypochondriasis and obsessive compulsive disorders.
HCL-15, a self-administered questionnaire, was developed by DJ Smith and his colleague in 2005 by modifying the HCL-32 into a 15 item checklist [21]. It issued to screen for a history of hypomanic symptoms by 15 yes/no items. The total score ranges from 0 to 15 with higher scores indicating more hypomanic symptoms. A cut-off greater or equal to 8 points is applied to define bipolar spectrum [21]. The English version of the HCL-15 was first translated into simplified Chinese by the author of this study, and then the back translation was performed by a bilingual psychiatrist who was unaware of the content of original HCL-15 [19]. The sensitivity of HCL- 15 in detecting BDII was 0.78 and 0.46 for BDI [19]. The Cronbach’s alpha value of the checklist was 0.94 based on the 653 patients in this study. We used the same cut-off of 8 point to define bipolar disorder.
HAMD-17 was used to evaluate the severity of depression [26]. We used this scale to reduce the bias from severity of depression when comparing BD and MDD.
▪ Statistical analyses
All of the data were analyzed by the Statistical Package for Social Science (SPSS) version 20.0. We used Univariate binary logistic regressions to find out potential variables which may distinguish BDI or BDII from MDD. Multivariate forward stepwise binary logistic regressions were then applied to control confounding and ascertain the independent related variables that were suggested by Univariate analyses. Age, gender and the score of HAMD-17 were forced into every multivariate analysis for controlling potential bias produced by sociodemographic factors and depression severity.
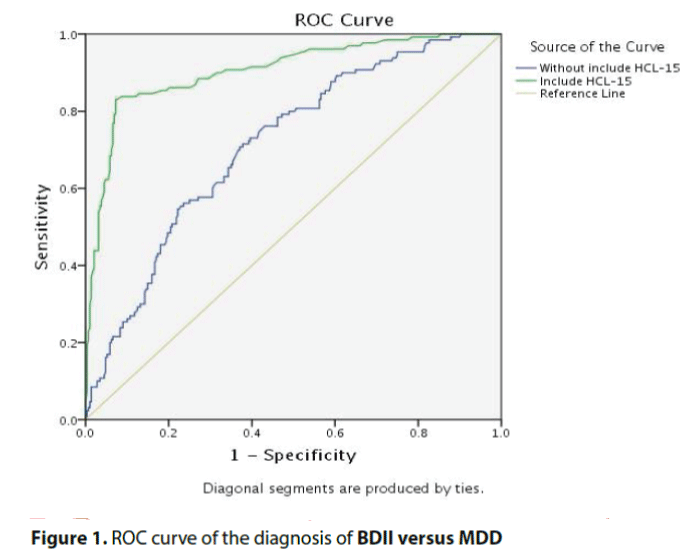
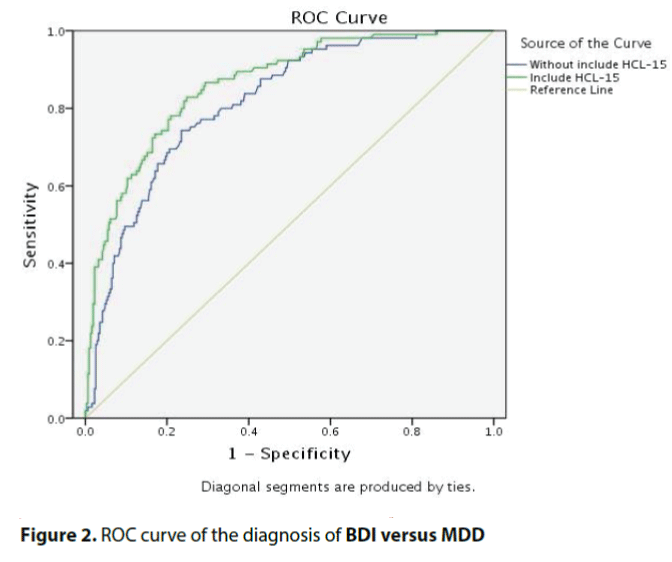
Receiver Operating Characteristic curves (ROC) were plotted based on the predictive values generated by the multivariate analyses. Areas under curves (AUC) were calculated to summarize the power of every multivariate analysis. Chi-square tests were performed to compare AUC of the models with and without the result of HCL-15. Statistically significant level was set at P ≤ 0.05 with two tails.
Results
▪ Description of subjects
A total of 713 consecutive patients were screened, with 78 of them unwilling or unsuitable to join the project. Finally, 635 patients (89.1%) were enrolled in the study, with 122 BD I, 160 BD II and 353 MDD. There were no significant differences of sociodemographic characteristics between participants and non-participants.
Table 1 shows the basic sociodemographic factors of the patients across diagnostic categories. Compared to patients with MDD, patients with BDI were less likely to be female, which was the only demographic feature difference finding between these two types of disorders. Compared to patients with MDD, patients with BDII were more likely to be younger, received more years of education, and to be divorced or never married.
| Characteristic | BDI(n=122) | BDII(n=160) | BD(n=282) | MDD(n=353) | BDI versus MDD OR 95%CI |
BDII versus MDD | BD versus MDD | |||
| n (%) | n (%) | n (%) | n (%) | OR | 95%CI | OR | 95%CI | |||
| Sex: female | 48(39.3) | 87(54.4) | 135(47.9) | 201(56.9) | 0.49** | 0.32-0.75 | 0.90 | 0.62-1.31 | 0.69* | 0.51-0.95 |
| Marital status | ||||||||||
| Married/cohabiting | 57(46.7) | 67(41.9) | 124(44.0) | 202(57.2) | 1.00 | 1.00-1.00 | 1.00 | 1.00-1.00 | 1.00 | 1.00-1.00 |
| Divorced/separated/widowed | 9(7.4) | 12(7.5) | 21(7.4) | 15(4.2) | 2.13 | 0.89-5.11 | 2.41* | 1.08-5.41 | 2.28* | 1.13-4.59 |
| Never married | 56(45.9) | 81(50.6) | 137(48.6) | 136(38.5) | 1.46 | 0.95-2.24 | 1.80** | 1.21-2.65 | 1.64** | 1.18-2.27 |
| Occupation | ||||||||||
| Full time job | 52(42.6) | 64(40.0) | 116(41.1) | 140(39.7) | 1.00 | 1.00-1.00 | 1.00 | 1.00-1.00 | 1.00 | 1.00-1.00 |
| Part-time job | 6(4.9) | 8(5.0) | 14(5.0) | 30(8.5) | 0.54 | 0.21-1.37 | 0.58 | 0.25-1.34 | 0.56 | 0.28-1.11 |
| Retire/unemployed | 64(52.5) | 88(55.0) | 152(53.9) | 183(51.8) | 0.94 | 0.61-1.44 | 1.05 | 0.71-1.55 | 1.00 | 0.72-1.39 |
| Personal income (RMB) | ||||||||||
| Above 10000 | 2(1.6) | 4(2.5) | 6(2.1) | 10(2.8) | 1.00 | 1.00-1.00 | 1.00 | 1.00-1.00 | 1.00 | 1.00-1.00 |
| 3000-9999 | 20(16.4) | 24(15.1) | 44(15.7) | 44(12.5) | 2.27 | 0.46-11.34 | 1.36 | 0.39-4.82 | 1.67 | 0.56-4.98 |
| 500-2999 | 42(34.4) | 49(30.8) | 91(32.4) | 151(43.0) | 1.39 | 0.29-6.60 | 0.81 | 0.24-2.70 | 1.00 | 0.35-2.86 |
| Below 499 | 58(47.5) | 82(51.6) | 140(49.8) | 146(41.6) | 1.99 | 0.42-9.34 | 1.40 | 0.43-4.62 | 1.60 | 0.57-4.51 |
| Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | |||||||
| Age, years | 33.0(12.1) | 32.0(12.5) | 32.4(12.3) | 35.6(13.2) | 0.98 | 0.97-1.00 | 0.98** | 0.96-0.99 | 0.98** | 0.97-0.99 |
| Years of education | 11.7(4.0) | 12.2(4.3) | 12.0(4.2) | 10.9(4.1) | 1.04 | 1.00-1.10 | 1.08** | 1.02-1.12 | 1.06** | 1.02-1.11 |
BDI=bipolar I disorder; BDII=bipolar II disorder; BD=BDI+BDII; MDD=major depressive disorder; OR=odd ratio; CI=confidence interval
a by univariate logistic regression. *P<0.05, **P<0.01;
Table 1: Comparison of sociodemographic features of BDI, BDII, BD and MDD patientsa.
▪ Clinical features
Patients with BD (BDI+BDII) experienced their first mood episode 5 years earlier than those with MDD,
Compared to patients with MDD, BDI patients were more likely to manifest psychotic features, to be obesity/overweight, and to receive hospitalization admissions. Compared to MDD patients, BDII patients were more likely to experience seasonal depressive onset, had more mixed depression. (Table 2)
| BDI(n=122) | BDII(n=160) | BD(n=282) | MDD(n=353) | BDI versus MDD ORb 95%CI |
BDII versus MDD | BD versus MDD | ||||
| n(%) | n(%) | n(%) | n(%) | OR | 95%CI | OR | 95%CI | |||
| Early onset(<25 years) | 67(54.9) | 98(61.2) | 165(58.5) | 146(41.4) | 1.72** | 1.14-2.62 | 2.24** | 1.53-3.28 | 2.00** | 1.46-2.75 |
| Precipitating factors before onset | 39(32.5) | 62(39.5) | 101(36.5) | 157(45.0) | 0.59* | 0.38-0.91 | 0.80 | 0.54-1.17 | 0.70* | 0.51-0.97 |
| Family history of BD | 26(22.6) | 34(23.0) | 60(22.8) | 43(13.1) | 1.93* | 1.12-3.32 | 1.97** | 1.20-3.25 | 1.95** | 1.27-3.00 |
| Seasonal depressive onset | 2(1.7) | 7(4.7) | 9(3.4) | 2(0.6) | 2.89 | 0.40-20.78 | 8.11** | 1.67-39.56 | 5.79* | 1.24-27.05 |
| Psychotic feature | 50(41.0) | 42(26.2) | 92(32.6) | 1.6(30.0) | 1.62* | 1.06-2.48 | 0.83 | 0.55-1.26 | 1.13 | 0.81-1.58 |
| Catatonic feature | 3(2.5) | 7(4.4) | 10(3.5) | 11(3.1) | 0.78 | 0.22-2.86 | 1.42 | 0.54-3.74 | 1.14 | 0.48-2.73 |
| Melancholic feature | 52(42.6) | 78(48.8) | 130(46.1) | 163(46.2) | 0.87 | 0.57-1.31 | 1.11 | 0.76-1.61 | 1.00 | 0.73-1.37 |
| Atypical feature | 30(24.6) | 43(26.9) | 73(25.9) | 84(23.8) | 1.04 | 0.65-1.69 | 1.18 | 0.77-1.80 | 1.12 | 0.78-1.61 |
| Mixed depression | 17(13.9) | 25(15.8) | 42(15.0) | 28(8.0) | 1.87 | 0.99-3.56 | 2.18** | 1.22-3.87 | 2.04 | 1.23-3.39 |
| Obesity/overweight | 33(27.0) | 28(17.5) | 61(21.6) | 47(13.3) | 2.41** | 1.46-4.00 | 1.38 | 0.83-2.30 | 1.80** | 1.19-2.73 |
| Comorbidity of anxiety disorders | 58(47.5) | 94(59.1) | 152(54.1) | 201(57.1) | 0.68 | 0.45-1.03 | 1.09 | 0.74-1.59 | 0.89 | 0.65-1.21 |
| Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | |||||||
| Age at first onset, years | 26.0(10.3) | 24.9(11.4) | 25.4(11.0) | 30.3(13.2) | 0.97** | 0.95-0.99 | 0.96** | 0.95-0.98 | 0.97** | 0.95-0.98 |
| Number of total episodes | 4.5(3.7) | 2.9(1.6) | 3.6(3.4) | 2.3(1.8) | 1.57** | 1.36-1.80 | 1.25** | 1.11-1.41 | 1.49** | 1.32-1.68 |
| Number of hospitalization | 2.1(1.4) | 1.5(1.0) | 1.8(1.3) | 1.6(1.4) | 1.32** | 1.09-1.59 | 0.93 | 0.75-1.15 | 1.14 | 0.97-1.35 |
BDI=bipolar I disorder; BDII=bipolar II disorder; BD=BDI+BDII; MDD=major depressive disorder; OR=odd ratio; CI=confidence interval
aby univariate logistic regression. *P<0.05, **P<0.01;
Table 2: Comparisons of clinical features of BDI, BDII, BD and MDD patientsa.
▪ Current and past symptoms
As shown in Table 3, the following depressive symptoms were found to be less-represented in BDI versus MDD: diminished interest, decreased appetite and fatigue, while symptoms of Irritable mood and talkativeness were more seen in BDI versus MDD. In contrast to the BDI comparisons, only one current manic symptomsirritable mood- was found more prevalent in BDII, and no significant differences were found upon depressive symptoms.
| Depressive symptoms | BDI(n=122) | BDII(n=160) | BD(n=282) | MDD(n=353) | BDI versus MDD OR 95%CI |
BDII versus MDD | BD versus MDD | |||
| n(%) | n(%) | n(%) | n(%) | OR | 95%CI | OR | 95%CI | |||
| Depressed mood | 121(99.2) | 158(99.4) | 279(99.3) | 350(99.4) | 0.69 | 0.06-7.69 | 0.90 | 0.08-10.03 | 0.80 | 0.11-5.70 |
| Diminished interest | 97(79.5) | 146(91.8) | 243(86.5) | 322(91.5) | 0.36** | 0.20-0.64 | 1.05 | 0.53-2.06 | 0.60* | 0.36-0.99 |
| Increased appetite | 2(1.7) | 4(2.5) | 6(2.1) | 4(1.1) | 1.46 | 0.26-8.09 | 2.24 | 0.55-9.09 | 1.91 | 0.53-6.82 |
| Decreased appetite | 68(55.7) | 107(67.3) | 175(62.3) | 234(66.5) | 0.64* | 0.42-0.97 | 1.04 | 0.70-1.55 | 0.83 | 0.60-1.15 |
| Weight lost | 58(47.5) | 94(59.1) | 152(54.1) | 192(54.5) | 0.76 | 0.50-1.14 | 1.21 | 0.83-1.76 | 0.98 | 0.72-1.35 |
| Insomnia | 87(71.3) | 112(70.4) | 199(70.8) | 258(73.5) | 0.90 | 0.57-1.42 | 0.86 | 0.57-1.30 | 0.88 | 0.62-1.24 |
| Psychomotor agitation | 85(69.7) | 116(72.5) | 201(71.3) | 255(72.2) | 0.88 | 0.56-1.39 | 1.01 | 0.67-1.54 | 0.95 | 0.67-1.35 |
| Psychomotor retardation | 109(89.3) | 151(94.4) | 260(92.2) | 333(94.3) | 0.50 | 0.24-1.05 | 1.00 | 0.45-2.27 | 0.71 | 0.38-1.33 |
| Fatigue | 99(81.1) | 142(89.3) | 241(85.8) | 315(89.5) | 0.51* | 0.29-0.89 | 0.98 | 0.53-1.80 | 0.71 | 0.44-1.14 |
| Worthlessness | 79(64.8) | 117(73.6) | 196(69.8) | 250(71.0) | 0.75 | 0.48-1.16 | 1.14 | 0.75-1.73 | 0.94 | 0.67-1.33 |
| Diminished ability to think or concentrate |
80(65.6) | 119(74.8) | 199(70.8) | 256(72.7) | 0.71 | 0.46-1.11 | 1.12 | 0.73-1.71 | 0.91 | 0.64-1.29 |
| Thoughts of death | 69(56.6) | 92(57.9) | 161(57.3) | 181(51.4) | 1.23 | 0.81-1.86 | 1.30 | 0.89-1.89 | 1.27 | 0.93-1.74 |
| Inside depression hypomania symptoms | ||||||||||
| Distractibility | 86(70.5) | 130(81.8) | 216(76.9) | 273(77.6) | 0.69 | 0.44-1.10 | 1.30 | 0.81-20.8 | 0.96 | 0.66-1.40 |
| Racing/crowded thought | 12(9.9) | 15(9.4) | 27(9.6) | 29(8.2) | 1.23 | 0.61-2.49 | 1.16 | 0.60-2.23 | 1.19 | 0.69-20.6 |
| Irritable mood | 45(37.2) | 65(40.9) | 110(39.3) | 91(25.9) | 1.70* | 1.10-2.64 | 1.98** | 1.34-2.95 | 1.86** | 1.32-2.60 |
| More talkativeness | 10(8.3) | 8(5.0) | 18(6.4) | 13(3.7) | 2.35* | 1.00-5.51 | 1.38 | 0.56-3.40 | 1.79 | 0.86-3.72 |
| Increased risky activities | 6(5.0) | 9(5.7) | 15(5.4) | 14(4.0) | 1.26 | 0.47-3.36 | 1.45 | 0.61-3.42 | 1.37 | 0.65-2.88 |
| Increased goal directed activity | 3(2.5) | 0(0) | 3(1.1) | 3(0.9) | 2.96 | 0.59-14.85 | 0.0 | 0.00-0.00 | 1.26 | 0.25-6.29 |
| Reduced need for sleep | 3(2.5) | 2(1.3) | 5(1.8) | 3(0.9) | 2.96 | 0.59-14.85 | 1.48 | 0.25-8.96 | 2.12 | 0.50-8.93 |
| Past hypomania symptom | ||||||||||
| Past hypomania symptoms(>=8) | 53(43.4) | 126(78.8) | 179(63.5) | 24(6.8) | 10.50** | 6.09-18.21 | 50.81** | 28.98-89.06 | 23.82** | 14.74-38.50 |
| Severity of depression | Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | ||||||
| HAMD-17 score | 26.1(7.0) | 27.3(6.3) | 26.9(6.4) | 27.1(6.3) | 0.98 | 0.95-1.01 | 1.01 | 0.98-1.04 | 0.99 | 0.97-1.02 |
BDI=bipolar I disorder; BDII=bipolar II disorder; BD=BDI+BDII; MDD=major depressive disorder; OR=odd ratio; CI=confidence interval;
aby univariate logistic regression. *P<0.05, **P<0.01;
Table 3: Comparisons ofdepressive and manic symptoms of BDI, BDII, BD and MDD patients.
There were no significant differences about HAMD-17 scores among three diagnostic groups. Compared to patients with MDD, both patients with BDI and BDII were more likely to get 8 or more scores in HCL-15.
▪Multivariate analyses with and without an inclusion of HCL-15
Without an inclusion of HCL-15
Compared to MDD, BDI diagnosis was significantly correlated with less female, more obesity/overweight, more total episodes, and less diminished interest symptoms, showing an AUC of 0.81(0.77-0.86). With regard to BDII versus MDD, a diagnosis of BDII was closely correlated with earlier age onset (before 25), more total episodes, more seasonal depressive onset, and more irritable mood symptoms, showing an AUC of 0.71 (0.66-0.77) (Table 4).
| Models | Independent variables | B | Wald | p | OR | 95%CI |
|---|---|---|---|---|---|---|
| BDI versus MDDa | Age | -0.02 | 2.35 | 0.125 | 0.98 | 0.96-1.01 |
| Gender(female) | -0.83 | 9.71 | 0.002 | 0.44 | 0.26-0.74 | |
| HAMD-17 | 0.00 | 0.00 | 0.959 | 1.00 | 0.96-1.04 | |
| Total episodes | 0.44 | 37.41 | <0.001 | 1.55 | 1.35-1.79 | |
| Obesity/overweight | 0.82 | 6.08 | 0.014 | 2.26 | 1.18-4.32 | |
| Diminished interest | -0.80 | 5.23 | 0.022 | 0.45 | 0.23-0.89 | |
| BDII versus MDDb | Age | 0.00 | 0.10 | 0.757 | 1.00 | 0.97-1.02 |
| Gender(female) | -0.12 | 0.28 | 0.597 | 0.88 | 0.56-1.40 | |
| HAMD-17 | 0.03 | 3.03 | 0.082 | 1.03 | 1.00-1.07 | |
| Seasonal depressive onset | 1.97 | 5.06 | 0.024 | 7.16 | 1.29-39.75 | |
| Irritable mood | 0.86 | 12.78 | <0.001 | 2.37 | 1.48-3.81 | |
| Total episodes | 0.18 | 7.61 | 0.006 | 1.20 | 1.05-1.36 | |
| Early onset(<25 years) | 0.80 | 6.13 | 0.013 | 2.21 | 1.18-4.16 |
BDI=bipolar I disorder; BDII=bipolar II disorder; MDD=major depressive disorder; OR=odd ratio; CI=confidence interval OR>1: less prevalent in MDD OR<1: more prevalent in MDD
aNagelkerke R Square=0.27, bNagelkerke R Square=0.14,
Table 4: Multivariate binary logistic regression models for BDI, BDII and BD versus MDD respectively (without include HCL-15).
With an inclusion of HCL-15
The results of the HCL-15 were added into the stepwise logistic models. Comparing BDI versus MDD, apart from the four features aforementioned, one independent predictor, which was eight past hypomanic symptom above, was identified, showing an AUC of 0.86(0.82-0.90) While in the comparison of BDII versus MDD, two features-more seasonal depressive onset and over eight past hypomanic symptoms above-were found, showing an AUC of 0.90 (0.87-0.94). The other four predictors aforementioned were excluded from the model (Table 5).
| Models | Independent variables | B | Wald | p | OR | 95%CI |
|---|---|---|---|---|---|---|
| BDI versus MDDa | Age | -0.02 | 1.78 | 0.182 | 0.98 | 0.96-1.01 |
| Gender(female) | -0.79 | 7.33 | 0.007 | 0.48 | 0.26-0.80 | |
| HAMD-17 | -0.00 | 0.00 | 0.941 | 1.00 | 0.96-1.04 | |
| Total episodes | 0.36 | 22.45 | <0.001 | 1.43 | 1.24-1.66 | |
| Obesity/overweight | 0.84 | 5.39 | 0.020 | 2.31 | 1.14 4.69 | |
| Diminished interest | -0.85 | 4.81 | 0.028 | 0.43 | 0.20-0.91 | |
| Past hypomania symptomd | 2.27 | 46.41 | <0.001 | 9.71 | 5.05-18.67 | |
| BDII versus MDDb | Age | -0.03 | 3.67 | 0.055 | 0.97 | 0.95-1.00 |
| Gender(female) | 0.10 | 0.09 | 0.761 | 1.11 | 0.57-2.17 | |
| HAMD-17 | 0.01 | 0.15 | 0.69 | 1.01 | 0.96-1.07 | |
| Seasonal depressive onset | 3.17 | 11.86 | 0.001 | 23.76 | 3.92-144.15 | |
| Past hypomania symptomd | 4.14 | 148.76 | <0.001 | 62.58 | 32.19-121.65 | |
| Constant | -1.92 | 9.85 | 0.002 | 0.15 | ||
BDI=bipolar I disorder; BDII=bipolar II disorder; MDD=major depressive disorder; OR=odd ratio; CI=confidence interval OR>1: less prevalent in MDD OR<1: more prevalent in MDD
aNagelkerke R Square=0.42, bNagelkerke R Square=0.64, dgreater or equal to 8 score base on HCL-15.
Table 5: Multivariate logistic regression models for BDI, BDII and BD versus MDD respectively (include HCL-15).
▪ Comparisons of AUCs of the models with and without the HCL-15
The inclusion of HCL-15 significantly increased the AUC of the model distinguishing BDII from MDD (0.90 versus 0.71, χ2=38.7, P<0.001). No significant difference was found between the comparisons of BDI versus MDD (Figures 1 and 2).
Discussion
To our knowledge, this is the first study to provide an evaluation of clinical features, current symptoms, and past hypomanic symptoms among BDI, BDII and MDD in Chinese clinical population. We found that: (1) most of the clinical features identified were consistent with the results from western studies; (2) three current depressive symptoms and two intro-MDE hypomanic symptoms were found different between BDI and MDD, whereas the comparison of BDII versus MDD yielded very few differences about current symptomatology; around 80% of patients with BDII and over 40% of patients with BDI self-reported to have at least 8 items of past hypomanic symptoms, while the figure was less than 7% in patients with MDD; 3) clinical features and current symptoms together showed good ability to distinguish BDI from MDD; however, they were not robust enough to discriminate BDII from MDD; (4) combining the result of HCL-15, clinical features and current symptoms significantly increased the power to distinguish BDII from MDD, but this was not the case for BDI versus MDD.
In Univariate analyses, most of the clinical features identified were consistent with previous studies. For example, compared to MDD, patients with BDI were more likely to have early onset [6,10-12], family history of BD [12,27,28], psychotic feature [10,14,29], more total episodes [10,13] and less trigger factors before onset [10,14]; patients with BDII had earlier onset [12], more family history of BD [6], more seasonal onset [15], and more mixed depression [11]. These factors seemingly did not change across the eastern and western cultures. In agreement with prior studies, the most salient differences in current symptoms were between BDI and MDD. Three depressive symptoms-diminished interests, decreased appetite, fatigue-were less prevalent in BDI patients, and more talkativeness and irritable mood were more prevalent in BDI. These results suggest that patients with BDI, even in severe depression, may be more likely to keep interest, appetite as well as energy compared with MDD counterparts. In line with a recent study [23], the comparison between BDII and MDD about current symptoms yielded very few differences, which means that it is very difficult to distinguish bipolar II depression from MDD by current symptomatology. On the one hand, the clinical features found from comparing BDII with MDD may indicate the bipolarity of BDII; on the other hand, the negative findings of current depressive symptoms may suggest the intermediary role of BDII across the BD-MDD spectrum.
Previous studies have shown that atypical features may be an important marker for BD and for BDII in particular [27]. Perhaps surprisingly, the differentiating function of atypical features was not repeated in this study. This inconsistent finding is probably due to sample difference. It was reported that atypical features may be more common in less severe depressive episodes [13]. However, most of the patients in our study were suffering from severe depressive episode (evaluated through HAMD-17), which might lower the possibility to manifest atypical features. Moreover, negative findings about atypical features in identifying BD were also reported in two recent studies [13,14]. Hence, whether atypical features are helpful in distinguishing BD from MDD, especially for those in severe depression, remains to be seen.
According to current diagnostic criteria, the difference between BD and MDD is based on lifetime presence or absence of manic/hypomanic symptoms. Detecting past hypomanic symptoms in depressive patients is crucial and usually viewed as a big challenge in clinical practice, especially for those with BDII. Our study, by using HCL-15, a past hypomanic checklist, showed that around 80% of patients with BDII and over 40% of patients with BDI self-reported to have at least 8 items of past hypomanic symptoms, while the figure was less than 7% in patients with MDD, which indicates that patients with BD, although in severe depression, still maintain the memory regarding past hypomanic experience. If they were systematically evaluated, either by using HCL-15 or by careful history taking, it is very likely to get enough information needed to make a diagnosis about BD.
To evaluate the combinative effect of clinical features, current symptoms and past hypomanic symptoms. We conducted multivariate logistic analyses with and without an inclusion of the result of HCL-15. When the result of HCL-15 were NOT put into the models, four independent factors-less female, more total episode, more obesity/overweight, less diminished interest-were found related to BDI, showing a good capacity to distinguish BDI from MDD(AUC=0.81,0.77-0.86). This figure was parallel to the result of a recent study, which obtained such effect by seven distinguishing features [23]; however, only four variables are needed in our model. The strongest factor with BDI in our sample was overweight/ obesity. Higher prevalence of obesity has been reported both in BD and MDD in comparison with general population [30,31]. We found, for the first time, that it might service as a distinguishing feature for BDI versus MDD. Indeed, overweight/obesity may be the result of frequently binge eating relate to the bipolar nature [32],or, just reflecting the consequence of the deleterious side effect of mood stabilizers and atypical antipsychotic commonly prescribed in BD patients [33]. Unfortunately, as information about medication was not included, the cause relationship is beyond this study. Further study in drug naive BD and MDD may contribute to answer this question. In any case, clinicians should be alert when treating patients with depression who have the problem of overweight/obesity. Other important differences we identified were consistent with previous studies, where patients with BDI were more likely to be male, and have more total episodes [6,10]. One current symptoms-diminished interestwas identified. This differed from the results of Leonpacher’s study, which has shown that psychomotor retardation, suicide behavior, psychotic symptoms and overall incapacity were more seen in BDI compare to MDD. As the author stated, those symptoms generally indicate a pattern of greater severity of depression. The patients in our study, however, were suffering from equally severe depression across three diagnostic categories, and we controlled the severity of depression by forcing the result of HAMD-17 into the multiple logistic analyses, which might exclude those depressive symptoms from the finial model.
Four variables survived in the multivariate regression model of BDII versus MDD, providing an AUC of 0.71(0.66-0.77). Seasonal depressive onset was the major contributor, followed by irritable mood, a kind of mixed symptom. Seasonal pattern of depressive episode was reported to be different between BD and MDD, and MDD patients with mixed feature tended to have similar seasonal pattern as that of BD patients [34,35]. Moreover, a recent study based on Chinese population also found seasonal depressive onset more prevalent in BDII compare to MDD [15]. Consequently, seasonality plus mixed symptoms might be associated with bipolarity in some extent. In accordance with recent studies, the comparison between BDII and MDD covering clinical features and current symptoms only provided fair ability to identify BDII [23], implying that merely using clinical features and current symptoms may not be an ideal way to detect BDII in patients with MDE.
When adding the result of HCL-15 to the models, the AUC of BDII versus MDD increased from 0.71 to 0.90, while there was no significant change of AUC in differentiating BDI from MDD. Focusing more on the symptoms of hypomanic activities rather than euphoria mood is one of the major changes of DSM-5 compare to DSM-IV in diagnosing hypomanic episode. The HCL-15, which is derived from HCL-32, is consisted of 15 items about hypomanic experiences, most of which are related to hypomanic behavior, while only one item is associated with elevated mood [19]. It may be easier for patients to recall the experience of past hypomanic behavior rather than that of elevated mood. Our study indicates that applying clinical features and HCL-15 together would be more helpful to distinguish BDII from MDD than using clinical features alone. Given that BDII is more likely to be misdiagnosed as MDD and receive antidepressant monotherapy, which may lead to worse clinical outcome [36], HCL-15 is highly suggested as an aided tool in clinical practice. Interestingly, as mentioned earlier, previously studies revealed that both HCL-32 [17,18,37] and MDQ [16] did not show better capacity in detecting BDII comparing to BDI, no matter in western or in Asian sample. The reason why HCL-15 can identify BDII better than BDI is unclear; direct comparisons of psychometric property between HCL-32 and HCL-32/MDQ is needed in the future.
This study has two major strengths. First, all of the patients underwent standardized diagnostic procedure, and we evaluated the current symptoms strictly according to the SCIDI/ P. Second, the severity of depression was evaluated by HAMD-17, and therefore may reduce the bias produced by the severity of depression.
Some limitations should be noted when interpreting our results. First, the proportion of in- and out- patients was not known, and all of the patients were recruited from tertiary medical centers, which may impede the generalization of the findings to patients from community. Second, it is possible that some MDD patients, especially the young, still hold the risk of developing into BD; however, around 60% of the MDD patients aged over 30 and thus pass the peak age of BD onset. Moreover, unidentified BD patients in the MDD group would decrease rather than increase the possibility of detecting significant findings. Third, information about medication used was not collected, so the impact of medications cannot be ruled out. Fourth, the cross-sectional nature of the study. Prospective longitudinal studies are needed to confirm and extend the findings of our study in the future.
In summary, this study demonstrates that using clinical features and current symptoms can provide good overall ability to discriminate BDI from MDD, but not satisfied enough to identify BDII. A combination of clinical features and HCL-15, a simple past hypomanic checklist, provides excellent ability to distinguish BDII from MDD. Our results, therefore, may aid clinicians to identify both BDI and BDII from patients with MDD in clinical practice.
Competing Interests
The authors declare that they have no competing interests.
Authors’ Contributions
The study was conceptualized by GYX. The SCID-I/P evaluations were completed by YMD, and the independent clinical assessments were completed by HYOY. The analysis was carried out by XDC, supervised by GYX & KGL. The manuscript was drafted by XDC and critically revised by KGL, YBG & HAS. All authors read and approved the final manuscript.
Acknowledgements
The authors are grateful to Professor Michael Phillips and his colleagues in Shanghai Mental Health Center for their selfless help in the writing process of the paper.
Funding Sources
This study was funded by the Scientific and Technological Project of Guangzhou city (2007Z3- E0611) and the 2012-2015 National Key clinical Specialty Project (20120108) in China.
References
- Hirschfeld RM, Lewis L, Vornik LA. Perceptions and impact of bipolar disorder: how far have we really come? Results of the national depressive and manic-depressive association 2000 survey of individuals with bipolar disorder. J. Clin. Psychiatry64(2), 161-174 (2003).
- First MB, Spitzer RL, Robbert L, et al.Structured Clinical Interview for DSM-IV-TR Axis I Disorders-Patient Edition (SCID-I/P, 11/2002 revision).
- Matza LS, Rajagopalan KS, Thompson CL, et al. Misdiagnosed patients with bipolar disorder: comorbidities, treatment patterns, and direct treatment costs. J. Clin. Psychiatry 66(11), 1432-1440 (2005).
- Birnbaum HG, Shi L, Dial E, et al.Economic consequences of not recognizing bipolar disorder patients: a cross-sectional descriptive analysis. J. Clin. Psychiatry 64(10), 1201-1209 (2003).
- Shi L, Thiebaud P, McCombs JS. The impact of unrecognized bipolar disorders for patients treated for depression with antidepressants in the fee-for-services California Medicaid (Medi-Cal) program. J. Affect. Disord 82(3), 373-383 (2004).
- Moreno C, Hasin DS, Arango C, et al.Depression in bipolar disorder versus major depressive disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Bipolar. Disord 14(3), 271-282 (2012).
- Houenou J, Frommberger J, Carde S, et al.Neuroimaging-based markers of bipolar disorder: evidence from two meta-analyses. J. Affect. Disord132(3), 344-355 (2011).
- Ghaemi SN, Bauer M, Cassidy F, et al.Diagnostic guidelines for bipolar disorder: a summary of the International Society for Bipolar Disorders Diagnostic Guidelines Task Force Report. Bipolar. Disord10(), 117-128 (2008).
- Cardoso de Almeida JR, Phillips ML. Distinguishing between unipolar depression and bipolar depression: current and future clinical and neuroimaging perspectives. Biol. Psychiatry73(1-2), 111-118 (2013).
- Serretti A, Mandelli L, Lattuada E, et al.Clinical and demographic features of mood disorder subtypes. Psychiatry. Res112(3), 195-210 (2002).
- Benazzi F. Mixed depression: a clinical marker of bipolar-II disorder. Prog. Neuropsychopharmacol. Biol. Psychiatry29(2), 267-274 (2005).
- Perlis RH, Brown E, Baker RW, et al.Clinical features of bipolar depression versus major depressive disorder in large multicenter trials. Am. J. Psychiatry163(2), 225-231 (2006).
- Schaffer A, Cairney J, Veldhuizen S, et al.A population-based analysis of distinguishers of bipolar disorder from major depressive disorder. J. Affect. disord 125(), 103-110 (2010).
- Gan Z, Diao F, Wei Q, et al.A predictive model for diagnosing bipolar disorder based on the clinical characteristics of major depressive episodes in Chinese population. J. Affect. disord 134(1-3), 119-25 (2011).
- Xiang YT, Zhang L, Wang G, et al.Sociodemographic and clinical features of bipolar disorder patients misdiagnosed with major depressive disorder in China. Bipolar. Disord15(2), 199-205 (2013).
- Miller C. Sensitivity and specificity of the Mood Disorder Questionnaire for detecting bipolar disorder. J. Affect. disord81(2), 167-171 (2004).
- Angst J, Adolfsson R, Benazzi F, et al.The HCL-32: Towards a self-assessment tool for hypomanic symptoms in outpatients. J. Affect.Disord88(2), 217-33 (2005).
- Yang H-c, Yuan C-m, Liu T-b, et al. Validity of the 32-item Hypomania Checklist (HCL-32) in a clinical sample with mood disorders in China. BMC. Psychiatry11(1), 84 (2011).
- He H, Xu G, Sun B, et al.The use of 15-point hypomanic checklist in differentiating bipolar I and bipolar II disorder from major depressive disorder. Gen. Hosp. Psychiatry36(3), 347-351 (2014).
- Meyer TD, Hammelstein P, Nilsson L-G, et al.The Hypomania Checklist (HCL-32): its factorial structure and association to indices of impairment in German and Swedish nonclinical samples. Compr. Psychiatry48(1), 79-87 (2007).
- Smith DJ, Harrison N, Muir W, et al.The high prevalence of bipolar spectrum disorders in young adults with recurrent depression: toward an innovative diagnostic framework. J. Affect. disord84(2-3), 167-78 (2005).
- Li Z, Zhang C, Fan J, et al. Brain-derived neurotrophic factor levels and bipolar disorder in patients in their first depressive episode: 3-year prospective longitudinal study. Br. J. Psychiatry205:29-35 (2014).
- Leonpacher AK, Liebers D, Pirooznia M, et al.Distinguishing bipolar from unipolar depression: the importance of clinical symptoms and illness features. Psychol. Med45(11), 2437-2446 (2015).
- Xu G, Lin K, Rao D, et al.Neuropsychological performance in bipolar I, bipolar II and unipolar depression patients: a longitudinal, naturalistic study. J. Affect. Disord136(3), 328-39 (2012).
- Chen HZ. Practical Internal Medicine: People's Medical Publishing House (2001).
- Zhao JP, Zhen YP. The reliability and validity of the 17-items Hamilton Depression Scale(HAMD). Chin. Mental. Health. J6(1), 214-6 (1992).
- Akiskal HS, Benazzi F. Atypical depression: a variant of bipolar II or a bridge between unipolar and bipolar II? J. Affect.Disord 84(2-3), 209-217 (2005).
- Benazzi F. Symptoms of depression as possible markers of bipolar II disorder. Prog. Neuropsychopharmacol. Biol. Psychiatry30(3), 471-477 (2006).
- Mitchell PB, Wilhelm K, Parker G, et al.The clinical features of bipolar depression: a comparison with matched major depressive disorder patients. J. Clin. Psychiatry 62(3), 212-216 (2001).
- McIntyre RS, Konarski JZ, Wilkins K, et al.Obesity in bipolar disorder and major depressive disorder: results from a national community health survey on mental health and well-being. Can. J. Psychiatry 51(5), 274-280 (2006).
- Simon GE, Von Korff M, Saunders K, et al.Association between obesity and psychiatric disorders in the US adult population.Arch. Gen. Psychiatry63(7), 824-830 (2006).
- Wildes JE, Marcus MD, Fagiolini A. Obesity in patients with bipolar disorder: a biopsychosocial-behavioral model. J. Clin. Psychiatry67(6), 904-915 (2006).
- Susce MT, Villanueva N, Diaz FJ, et al. Obesity and associated complications in patients with severe mental illnesses: a cross-sectional survey. J. Clin. Psychiatry 66(2), 167-173 (2005).
- Shin K, Schaffer A, Levitt AJ, et al.Seasonality in a community sample of bipolar, unipolar and control subjects. J. Affect. Disord 86(1), 19-25 (2005).
- Sato T, Bottlender R, Sievers M, et al.Distinct seasonality of depressive episodes differentiates unipolar depressive patients with and without depressive mixed states. J. Affect. Disord90(1), 1-5 (2006).
- Singh T, Rajput M. Misdiagnosis of bipolar disorder. Psychiatry (Edgmont) 3(10), 57-63 (2006).
- Wu Y-S, Angst J, Ou C-S, et al. Validation of the Chinese version of the Hypomania Checklist (HCL-32) as an instrument for detecting hypo(mania) in patients with mood disorders. J. Affect. disord106(1-2), 133-143 (2008).