Research Article - (2018) Volume 8, Issue 6
Delayed Encephalopathy after Acute Carbon Monoxide Poisoning with Dynamic Progression of Radiologic and Clinical Manifestations
- Corresponding Author:
- Xue-Jun Liu
Department of Radiology, the Affiliated Hospital of Qingdao University, Qingdao, China
Tel: 8618661803701
E-mail: [email protected]
Abstract
Objective
To analyze retrospectively one case of delayed encephalopathy after acute carbon monoxide poisoning (DEACMP) that demonstrated both clinical and radiological progression and to summarize the experiences learned from the treatment of this case.
Method
Radiologic and clinical data from this case of DEACMP were reviewed.
Results
This patient had a normal C-reactive protein (CRP) level but an increased D-dimer level upon admission. A MRI scan of the brain indicated abnormal signals in the left thalamus and right centrum semiovale, along with mild abnormal signals in the bilateral symmetrical globus pallidus lesions (unfortunately, this sign was overlooked). He was initially diagnosed with cerebral infarction according to radiologic findings. After admission, the patient underwent symptomatic treatment and reexamination, and a routine blood test revealed an increased CRP level and a decreased D-dimer level. MRI scan revealed enlargement of the lesion in the right centrum semiovale, as well as new lesions in the bilateral parietal and occipital lobes. Based on clinical manifestations, a preliminary diagnosis of autoimmune encephalitis was made, and the patient’s conditions improved after symptomatic treatment. However, the symptoms were aggravated after lowering the hormone dose. Then he had another MRI scan, which revealed symmetrical signal abnormalities in the basal ganglia regions bilaterally and white matter around the posterior and anterior horns of lateral ventricles bilaterally. A normal CRP level was basically restored per a routine blood test, and the D-dimer level increased to 3580 ng/ml. According to clinical and radiological process, radiologist inquired the patient’s history, he admitted to having an explicit history of CO exposure. Therefore, the patient was finally diagnosed with DEACMP.
Conclusion
Early MRI findings of DEACMP may include atypical and asymmetric white matter lesions. Moreover, the signal abnormalities of the bilateral symmetrical globus pallidus lesions are not pronounced in the subacute stage and, therefore, may be easily neglected. Cerebral infarction may precede any white matter lesions. Laboratory tests including serum CRP and D-dimer levels can aid in the diagnosis of DEACMP.
Keywords
Carbon monoxide poisoning, Delayed neuropsychiatric sequelae, Magnetic resonance imaging, Clinical characteristics
Introduction
Acute carbon monoxide poisoning is a common poisoning related to occupational exposure or occurring in daily life, and it is more frequent in the rural areas of North China where current heating measures are antiquated. Delayed encephalopathy after acute carbon monoxide poisoning (DEACMP) is a common complication of the central nervous system following carbon monoxide poisoning. DEACMP usually presents as a series of neuropsychiatric symptoms and signs, typically dementia, after a false recovery lasting 2–60 days, following acute carbon monoxide poisoning [1,2]. However, the pathogenesis of DEACMP remains unclear. DEACMP has a high disability rate and mortality, longer-term exposure to carbon monoxide and older age, as well as a history of hypertension and arteriosclerosis, are risk factors for DEACMP [3,4]. Therefore, early diagnosis and timely treatment are crucial for the prognosis of patients with DEACMP. However, if the radiologic manifestations and clinical symptoms of DEACMP are atypical, and the patient did not mention a history of carbon monoxide exposure,inexperienced radiologists and physicians can easily make the wrong diagnosis. Therefore, mastering its pathogenesis, typical and atypical imaging manifestations, clinical symptoms, and laboratory examination indexes are of great significance for its early diagnosis and treatment. We analyzed a case of DEACMP with dynamic progression of radiologic and clinical manifestations retrospectively to summarized pathogenesis, imaging manifestations, clinical features of DEACMP to help improve the diagnosis of it.
Methods
The hospital ethics committee approved this retrospective study, and the need for obtaining informed consent from patients was waived. A 74-year-old man visited the emergency department at our hospital on December 5, 2016, because of dizziness with bilateral blurred vision and hearing loss for unknown reasons for 4 days. Radiologic and clinical data from this case of DEACMP were reviewed.
Results
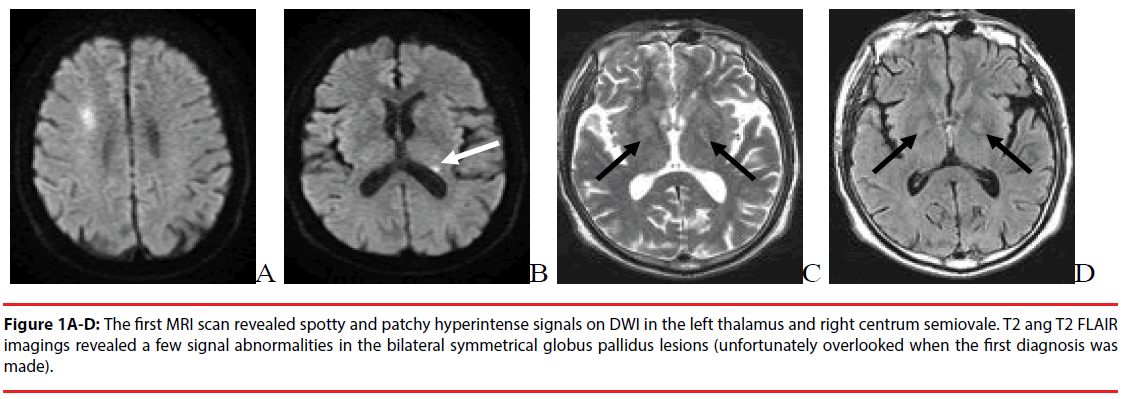
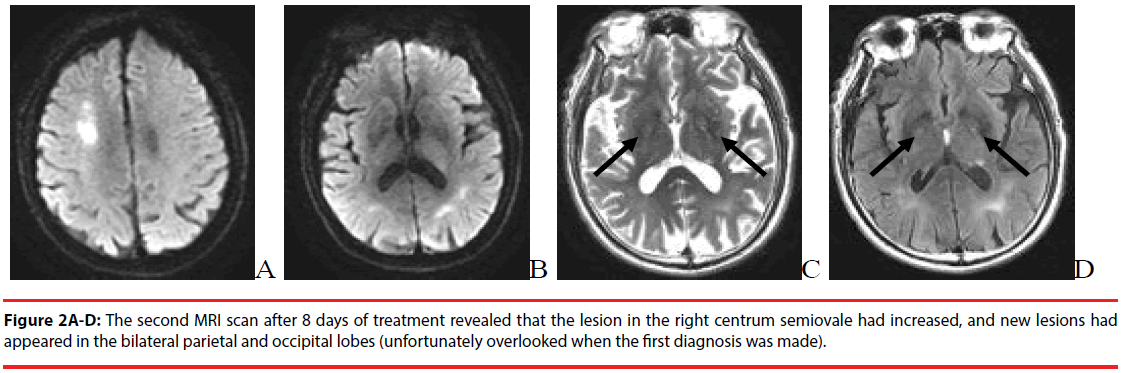
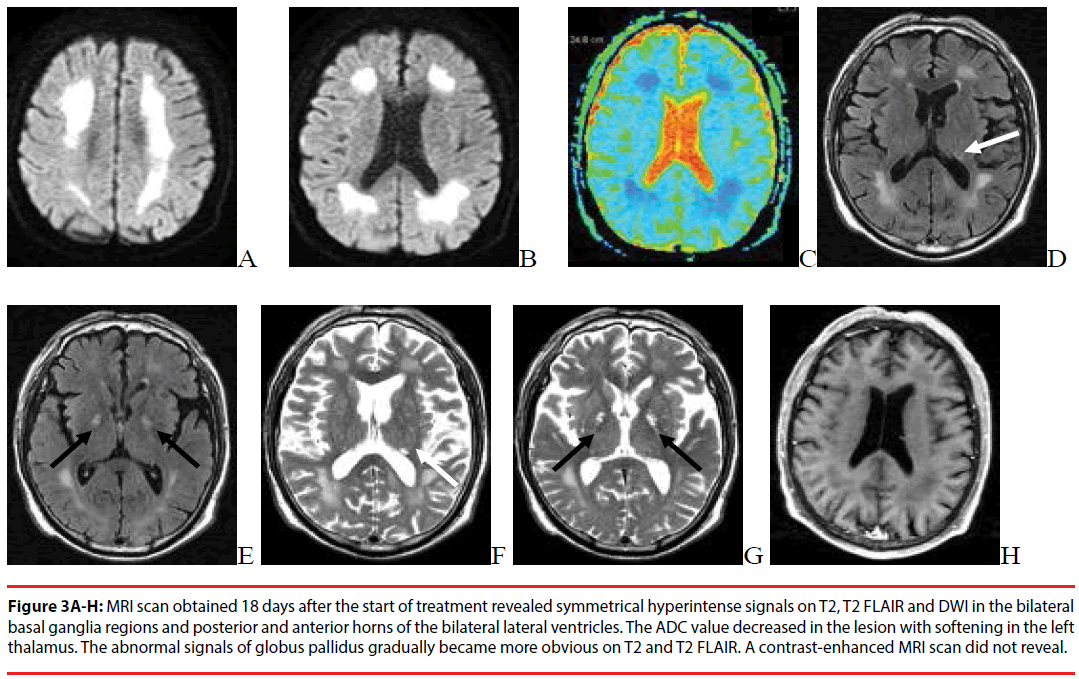
CT scan of the brain did not reveal any abnormalities. This patient was initially diagnosed with cerebral ischemia and administered symptomatic and supportive treatments including antithrombotic therapy and cerebral blood flow–improving therapy for 10 days. However, his symptoms had not improved, and the patient was re-hospitalized on December 14, 2016. A routine blood test showed a C-reactive protein (CRP) level of 4.24 mg/l, and a blood coagulation test showed a D-dimer level of 3380 ng/ml. No other abnormalities were found. MRI scan of the brain indicated multiple patchy signals in the left thalamus and right centrum semiovale (Figure 1A-D). MRA did not reveal any apparent abnormalities, and this patient was diagnosed with a cerebral infarction based on radiologic findings. After hospitalization, he was administered anticoagulation, lipid-lowering, and circulation-improving therapies for 4 days. His dizziness was relieved, but the patient still complained of bilateral blurred vision, hearing loss, fatigue, and an unsteady gait. Another routine blood test revealed a D-dimer level of 2090 ng/ml, which was lower than the result obtained on December 14, 2016. The abovementioned treatments were continued until December 21, 2016. However, the patient began to have symptoms of a cognitive dysfunction including an apathetic expression and slow reactions, with occasional incontinence. Further treatments were suggested, and tests were performed to exclude encephalitis, poisoning, and metabolic diseases. Another MRI scan of the brain was performed the next day that revealed an enlargement of the lesion in the right centrum semiovale, as compared with the scan obtained on December 14, 2016. A new lesion was discovered in the bilateral parietal and occipital lobes (Figure 2A-D). A blood coagulation test indicated that the D-dimer level decreased to 1870 ng/ml, but a routine blood test indicated an increase in the CRP level to 44.58 mg/l. Arteriosclerosis of the intracranial vessels was found using DSA without stenosis of the beginning portion of the internal carotid, and there were multiple irregular stenoses of the distal end of the internal carotid. A lumbar puncture was performed, and routine cerebrospinal fluid (CSF) and biochemistry tests indicated an increase in CSF proteins and immunoglobulins. Autoimmune encephalitis was suspected based on these findings. Impact therapy using 1 g of methylprednisolone was administered in combination with pantoprazole sodium to protect the stomach. In addition, anticoagulation, lipid-lowering, and circulationimproving treatments were administered. The patient’s symptoms improved after the treatment. The dose of hormones was decreased on January 1, 2017, but the symptoms were more pronounced and became as serious as before treatment. An additional MRI scan of the brain indicated symmetrical signal abnormalities in the bilateral basal ganglia regions and white matter around the posterior and anterior horns of the bilateral lateral ventricles. The ADC value of the lesion decreased, the abnormal signals of globus pallidus gradually became more obvious on T2, T2 FLAIR, and contrast-enhanced MRI did not reveal any conspicuous enhancement of the lesion. There was softening of the lesion in the left thalamus (Figure 3A-H). The CRP level was basically normal at this time, and the D-dimer level increased to 3580 ng/ml. The patient and their relatives were questioned about their medical history. It was found that the patient lived alone before disease onset and that he burned coal in a stove for heat during the winter. This patient had an explicit history of carbon monoxide exposure, and combined with his clinical manifestation, he was finally diagnosed with DEACMP. His symptoms improved after hyperbaric oxygen therapy and other abovementioned comprehensive symptomatic support therapy, and the patient was discharged.
Figure 1A-D: The first MRI scan revealed spotty and patchy hyperintense signals on DWI in the left thalamus and right centrum semiovale. T2 ang T2 FLAIR imagings revealed a few signal abnormalities in the bilateral symmetrical globus pallidus lesions (unfortunately overlooked when the first diagnosis was made).
Figure 3A-H: MRI scan obtained 18 days after the start of treatment revealed symmetrical hyperintense signals on T2, T2 FLAIR and DWI in the bilateral basal ganglia regions and posterior and anterior horns of the bilateral lateral ventricles. The ADC value decreased in the lesion with softening in the left thalamus. The abnormal signals of globus pallidus gradually became more obvious on T2 and T2 FLAIR. A contrast-enhanced MRI scan did not reveal.
Discussion
Carbon monoxide poisoning mainly affects the cerebral cortex, globus pallidus, thalamus, and corpus striatum [5]. Once these functional areas become involved, patients will experience cognitive dysfunction, ncontinence, an unsteady gait, Parkinson’s disease, and psychotic symptoms [6]. The bilateral symmetrical globus pallidus lesions are considered the characteristic manifestations during the acute stage of carbon monoxide poisoning. Symmetrical white matter lesions in the bilateral lateral ventricles are typical of DEACMP [7]. Our patient’s disease course progressed from the initial symptoms of dizziness, blurred vision, and hearing loss to cognitive dysfunction. Progressive white matter lesions were observed radiologically. However, the typical symptoms of acute carbon monoxide poisoning or radiologic findings of DEACMP were absent during the early stages of the disease. This is probably because the patient was not administered any special treatment immediately after acute carbon monoxide poisoning because of mild symptoms. When the symptoms appeared and the patient was hospitalized, he was between the acute stage of carbon monoxide poisoning and peak stage of DEACMP. The first CT scan did not reveal any abnormal lesions in the brain. However, his symptoms progressed after hospitalization. The first MRI scan on the ninth day after hospitalization revealed hyperintense signals in the white matter of the right centrum semiovale and left thalamus on DWI (the lesion in the right centrum semiovale was misdiagnosed as a cerebral infarction). The second MRI scan on the 18th day after hospitalization indicated asymmetrical white matter lesions in the bilateral lateral ventricles. Coupling the laboratory test results with his symptoms, this patient was finally diagnosed with autoimmune encephalitis. It was not until the third MRI scan on the 13th day after hospitalization that the symmetrical white matter lesions in the bilateral lateral ventricles were found. This was typical of poisoning/metabolic diseases, combining these findings with the patient’s medical history, his final diagnosis was confirmed to be DEACMP. It should be noted that the symmetrical globus pallidus lesions typical of acute carbon monoxide poisoning were not conspicuous during several radiologic scans. In contrast, these lesions appeared as mild signal abnormalities in the MRI scans (indicated by blank arrowheads in Figure 1C-D and 2CD). The probable reason is that the patient was treated in a non-acute stage of carbon monoxide poisoning when the cytotoxic edema related to the globus pallidus lesions had evolved into necrotic repair during a subacute stage. This led to a “blurring effect” which is similar to cerebral infarction,making the symmetrical globus pallidus lesions revealed inconspicuously in the MRI scans. Unfortunately, the physicians overlooked this sign during diagnosis. However, such atypical radiologic symptoms of DEACMP were very rare in the clinic, and the patient did not mention a history of carbon monoxide exposure. Inexperienced radiologists and physicians can easily make the wrong diagnosis in this situation.
The pathogenesis of DEACMP still remains unclear, and most scholars attribute the cause to secondary vascular lesions. After carbon monoxide poisoning, the cerebral vessels first experience spasm and then dilation with an increase in permeability. Cellular degeneration of the vascular wall will lead to cerebral hypoxia and cerebral edema, as well as softening or necrosis of the globus pallidus and demyelinating changes in the cerebral white matter [8]. The appearance of the abovementioned pathological changes takes some time. A false recovery may occur after patients awaken from a coma, followed by neuropsychiatric symptoms. A theory of “Microemboli” has been proposed to explain the pathogenesis [9]. Acute carbon monoxide poisoning can cause hypoxia and injury of the vascular endothelial cells. This further weakens the anticoagulation and vasomotion functions. Moreover, platelets are highly activated, and a high platelet level is maintained until the recovery stage. A rough vascular intima causes platelet accumulation and microembolus formation, leading to cerebral edema and necrosis and demyelination of nerve cells. In addition, cytotoxic injury, ischemia-reperfusion injury, free radical and calcium overload, excitatory amino acids and cell apoptosis, immune dysfunction, inflammatory factors, and neurotransmitter disorders have also been proposed as the pathogenesis of DEACMP [10-14]. In our case, the first MRI scan indicated a lesion in the left thalamus that later evolved into a softening lesion during subsequent MRI scans. This lesion was confirmed to be a lacunar infarction (indicated by white arrowheads in Figure 1B and 3D-F). In addition, the blood D-dimer level increased considerably at the beginning and then decreased that seemed to implicate the role of microemboli in DEACMP. The patient had two CRP tests, and both indicated a persistent increase that may imply a connection between DEACMP and inflammatory response. However, the abovementioned hypotheses need to be further tested.
MRI is a useful tool for the diagnosis and differential diagnosis of DEACMP. Typical MRI manifestations of DEACMP include: (1) bilateral symmetrical dot-like, patchy, or confluent lesions in the white matter of the lateral ventricles and centrum semiovale. The lesions are usually shown as hypointense signals on T1WI and hyperintense signals on T2WI [15-18]; and (2) ischemia or necrosis of the basal ganglia regions, typically in the bilateral globus pallidus and shown as long T1 and short T2 signals. Our case did not mention having a history of carbon monoxide exposure during the first visit, and the radiologic manifestations were atypical in the first scan. The mildly abnormal signals in the bilateral globus pallidus were overlooked, leading to the wrong diagnosis. As the disease progressed, the asymmetrical white matter lesions with a cerebral infarction evolved into the typical symmetrical white matter lesions seen in DEACMP, the abnormal signals of globus pallidus gradually became more obvious.
This patient initially presented with the symptoms of dizziness, blurred vision, and hearing loss that soon evolved into a cognitive dysfunction within a month. The patient’s conditions progressed after hospitalization. The D-dimer and CRP levels in the blood fluctuated during the disease course. The former first increased and then decreased, and the latter continued to increase. Combined with the radiologic findings, the microemboli caused by the coagulation abnormalities might have played a role during the early stages of DEACMP, but this effect gradually weakened over time. The inflammatory response might have played a more significant role in the progression of white matter lesions in the later stage of DEACMP. These features of radiologic and clinical progression in DEACMP provide valuable clues to understand the pathogenesis. Another study has shown that the degree of increase in the CRP level correlated significantly with the duration of hospitalization. The laboratory marker, CRP, is useful for assessing the severity of carbon monoxide poisoning and helps in the early prediction of DEACMP [19]. The D-dimer level is positively correlated with the severity of carbon monoxide poisoning. DEACMP can be suspected if the patient has an abnormal increase or another increase in the D-dimer level during false recovery following carbon monoxide poisoning [20].
In conclusion, the early radiologic manifestations of DEACMP may be atypical, including asymmetrical white matter lesions that progress over time, accompanying with cerebral infarcts. Signal abnormalities in the bilateral globus pallidus may be inconspicuous in DEACMP sometime after the acute stage of carbon monoxide poisoning and, therefore, are easily overlooked. Serum CRP and D-dimer levels are useful for the early diagnosis and prognostic assessment of DEACMP. In rural areas of North China where coal is burned for heating purposes during the winter, progressive exasperation of central nervous system disorders such as cognitive impairment, along with symmetrical or asymmetrical white matter lesions, may indicate DEACMP. It is necessary to determine whether a patient has a history of carbon monoxide exposure (e.g., burning coal in an open stove) and to measure the serum CRP and D-dimer levels to substantiate the diagnosis. Early interventions should be done to reduce brain injury and improve prognosis and quality of life.
Funding
This study was funded by Current Funding Sources: The people’s Livelihood Science and technology project of Qingdao City (17-3-3-18- nsh)
References
- Vander Weyden L, Voigt RM, Boonen S, et al. Delayed neurological syndrome after CO intoxication of elderly female.Tijdschrift. voor. Gerontology. En. Geriatrie 46(5), 290-295 (2015).
- Shprecher DR, Flanigan KM, Smith AG, et al. Clinical and diagnostic features of delayed hypoxic leukoencephalopathy. J. Neuropsychiatry. Clin. Neurosci 20(4), 473-477 (2008).
- Hu H, Pan X, Wan Y, et al. Factors affecting the prognosis of patients with delayed encephalopathy after acute carbon monoxide poisoning. Am. J. Emerg. Med 29(3), 261-264 (2011).
- Weaver LK, Valentine KJ. Carbon monoxide poisoning: risk factors for cognitive sequelae and the role of hyperbaric oxygen. Am. J. Respir. Crit. Care. Med 176(5), 491-497 (2007).
- Hara S, Mukai T, Kurosaki K, et al. Characterization of hydroxyl radical generation in the striatum of free-moving rats due to carbon monoxide poisoning, as determined by in vivo microdialysis. Brain Research 1016(2), 281-284 (2004).
- Zhang J, Wu H, Zhao Y. Therapeutic Effects of Hydrogen Sulfide in Treating Delayed Encephalopathy After Acute Carbon Monoxide Poisoning. Am. J. Ther 23(6), e1709-e1714 (2016).
- Sung YF, Chen MH, Peng GS. Generalized chorea due to delayed encephalopathy after acute carbon monoxide intoxication. Ann. Indian. Acad. Neurol 18(1), 108-110 (2015).
- Yamazaki Y. Delayed encephalopathy after carbon monoxide intoxication. Internal. Medicine 47(11), 1071-1072 (2008).
- Kofler S, Nickel T. Role of cytokines in cardiovascular diseases: a focus on endothelial responses to inflammation. Clinical. Science 108(3), 205-213 (2005).
- Hampson NB, Piantadosi CA, Thom SR. Practice recommendations in the diagnosis, management, and prevention of carbon monoxide poisoning. Am. J. Respir. Crit. Care. Med 186(11), 1095-1101 (2012).
- Gorman D, Drewry A, Huang YL. The clinical toxicology of carbon monoxide. Toxicology 7(1), 25-38 (2006).
- Lo WC, Chan JY, Tung CS. Carbon monoxide and metabotropic glutamate receptors in rat nucleus tractus solitarii: participation in cardiovascular effect. Eur. J. Pharmacol 454(1), 39-45 (2002).
- Chen HL, Chen PC, Lu CH, et al. Structural and cognitive deficits in chronic carbon monoxide intoxication: a voxel-based morphometry study. BMC Neurology 13(1), 129 (2013).
- Thom SR, Bhopale VM. Hyperbaric oxygen reduces delayed immune-mediated neuropathology in experimental carbon monoxide toxicity. Toxicol. Appl. Pharmacol 213(2), 152-159 (2006).
- Beppu T. The role of MR imaging in assessment of brain damage from carbon monoxide poisoning: a review of the literature. AJNR 35(4), 625-631 (2014).
- Vella S, Kreis R, Lovblad KO. Acute leukoencephalopathy after inhalation of a single dose of heroin. Neuropediatrics 34(2), 100-104 (2003).
- Keogh CF, Andrews GT, Spacey SD, et al. Neuroimaging features of heroin inhalation toxicity: "chasing the dragon. AJR 80(3), 847-850 (2003).
- Kudo K, Otsuka K, Yagi J, et al. Predictors for delayed encephalopathy following acute carbon monoxide poisoning. BMC. Emergency. Medicine 14(1), 3 (2014).
- Grieb G, Simons D, Schmitz L, et al. Glasgow Coma Scale and laboratory markers are superior to COHb in predicting CO intoxication severity. Burns 37(4), 610-615 (2011).
- Kado H, Kimura H, Murata T, et al. Carbon monoxide poisoning: two cases of assessment by magnetization transfer ratios and 1H-MRS for brain damage. Radiation Medicine 22(3), 190-194 (2004).