Research Article - Neuropsychiatry (2018) Volume 8, Issue 1
Berberine Prevents Cognitive Disorders Induced by Sepsis by Regulating the Inflammatory Cytokines, Oxidative Stress and Neuronal Apoptosis in Rat Brain
- *Corresponding Author:
- Guoji Zhu and Wenwen Xu
Department of Internal Medicine
Soochow University Affiliated Children’s Hospital
303 Jingde Road, Suzhou, Jiangsu 215003, P.R. China
(Tel) +86 512806935021
(Fax) +86 512806935021
Abstract
Sepsis is a life-threatening organ dysfunction caused by a dysregulated host response to infection and can cause a huge burden to whole families and to society in terms of medical costs. Cognitive disorders induced by sepsis are still exasperating problems in clinical research. This paper examines a new measure of berberine (BBR) in sepsis induced cognitive disorders based on CLP surgery. BBR is one of many extracts from Chinese traditional herbs and exhibits antidiabetic, anticancer and antioxidant activities in treating various clinical disorders. Whether BBR shows efficacy in improving survival rates and inhibiting the extent of cognitive disorders after sepsis was explored in this paper.The result revealed that BBR treatment significantly improved the survival rate and cognitive disorders in septic rats. Increased levels of antioxidant superoxide dismutase (SOD) and reduced levels of lipid peroxidation malondialdehyde (MDA) were exhibited in the serum and brain tissue of the BBR treatment group. Moreover, the inflammatory cytokine (IL-1β, IL-4, IL-6, TNF-α) levels in the brain tissue were all decreased in the BBR treatment group compared to those in the sepsis group. BBR also largely protected the cells from apoptosis in the cerebral cortex and hippocampal CA1 region. Overall, our results indicated that BBR exhibited protective effects on survival rate and cognitive disorders after sepsis by inhibiting the release of inflammatory cytokines, oxidative stress and neuronal apoptosis in brain tissue. Therefore, BBR is a potential drug that shows efficacy in avoiding death rates and cognitive disorder after sepsis.
Keywords
Berberine (BBR), Sepsis, Cognitive disorder, Inflammatory cytokines, Oxidative stress, Apoptosis
Introduction
to the Third Consensus Definitions of Sepsis in 2016, sepsis is termed a life-threatening organ dysfunction caused by a dysregulated host response to infection [1]. Over half of sepsis patients have encephalopathy, which is one of the most common causes of altered mental status in medical-surgical ICUs [2,3]. Sepsis patients have higher risks for long-term cognitive impairments, including deficits in visual and functional memory, alteration in visual-spatial abilities, and depressive and anxiety disorders [4]. These cognitive impairments have serious impacts on the life quality of patients. Moreover, there are limitations and difficulties in precisely evaluating the cognition and sensory functions in patients with sepsis [5]. Therefore, this disease enhances adverse effects on patients and lay huge financial burden on families and society.
Though increasing research has focused on the pathophysiology of sepsis, the precise mechanism of sepsis is still poorly understood. For invading pathogens, an overwhelming inflammatory response was triggered which further sepsis occurred [6]. Innate immune cells were activated by pathogen-associated molecules (e.g., endotoxin) and then immediately recruited and activated neutrophils and macrophages to clear bacteria and repair injured tissue [7]. In sepsis, massive release of pro-inflammatory cytokines, including interleukin (IL) and tumour necrosis factor (TNF-α), was identified which further trigger multiple cell death and organ dysfunction [8]. In addition, patients with sepsis are often exposed to an imbalance of oxidants and antioxidants, further promoting cell death as well as tissue damage in susceptible regions of the brain, including the hippocampus [9]. Therefore, the balanced levels of lipid peroxidation malondialdehyde (MDA) and antioxidant superoxide dismutase (SOD) are appropriate markers in estimating and quantifying the extent of oxidative damage. Except for oxidative stress, mitochondrial-mediated apoptotic pathways also play an important role in the pathogenesis of sepsis [10]. Thus, efficient therapies towards antioxidant stress and anti-apoptosis in the pathogenesis of sepsis were urgent in avoiding the cognitive impairment induced by sepsis.
Recently, many traditional herbs, including curcumin [11] and ginsenoside Rg1 [12], have proved effective in treating sepsis induced cognitive dysfunction through suppression of oxidative stress-related inflammation via different signalling pathways. Berberine (BBR), which can be isolated from a variety of plants (i.e., Coptidis chinensis Franch, Phellodendron chinense Schneid, etc.), exhibits anti-diabetic, anti-cancer and anti-oxidant activities in treating some clinical disorders [13]. During the research of sepsis, BBR could prevent intestinal mucosal barrier damage at the early phase of disease [14]. In 2016, Yuan Wang revealed that neutrophil tissue infiltration and multiorgan dysfunction induced by sepsis was partly attenuated by combination treatment with BBR and yohimbine [15]. Research on whether BBR treatment alone improves cognitive functions after sepsis is sparse and not well documented.
In this study, we aimed to evaluate the effect of BBR on cognitive deficits and the underlying mechanism induced by caecal ligation and puncture (CLP) in rats. The inflammation activities of cytokines, oxidative stress and apoptotic cells in the hippocampus CA1 region are all measured in this study.
Methods
▪ Animals and drug administration
Male Sprague-Dawley (SD) rats (250 g to 300 g, Shanghai Slac Laboratory Animal Co. Ltd) were used in this study. All of animals were maintained on standard cages with free access to pellet food and water under independent ventilation system at temperature of 25 ± 1℃ on a 12 h light/12 h dark cycle. All of the studies were guided by the Animal Center of Soochow University, and the animal treatment protocol was approved by the ethics committee of the institution.
All rats in the experiment were divided into five groups at random (n=10 per group): the control group (Con), CLP surgery group (CLP), CLP surgery with BBR (50 mg/kg) treatment group (CLP+BBR1), CLP surgery with BBR (100 mg/ kg) treatment group (CLP+BBR2), CLP surgery treatment with saline group (CLP + vehicle). Animals of the three treatment groups with BBR or saline received BBR or saline by intragastric administration for 5 consecutive days. BBR was dissolved in saline solution before administration and the same volume of BBR or saline was administered before the sepsis model established.
▪ Induction of sepsis by caecal ligation and puncture (CLP)
Clinical polymicrobial sepsis features can be mimicked by CLP surgery [16]. Briefly, the experimental rats were anaesthetized with 0.2% isoflurane and a small midline incision was made on the anterior abdomen of rats. The caecum was isolated and the caecal appendage was ligated tightly 25% distal to the ileocaecal valve with surgical silk thread. Double punctures were performed with an 18-gauge needle on the same side near and distal to the ligation. If there was a small amount of faecal material extruding from the puncture area, the caecum was returned to the abdominal cavity and the incision closed by silk surgery suture. All the rats were removed to the recovery cage after receiving an injection of normal saline subcutaneously. Con group rats were treated as described above except for ligation or puncture.
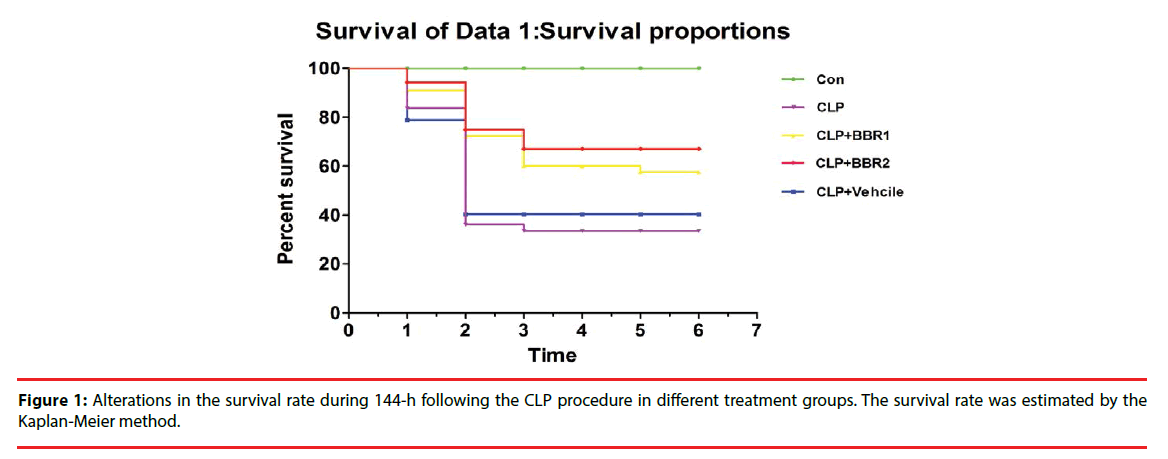
▪ Survival rate
The survival rates of the rats in the five groups were evaluated in 6 days after CLP surgery under normal cages which provided enough food and water.
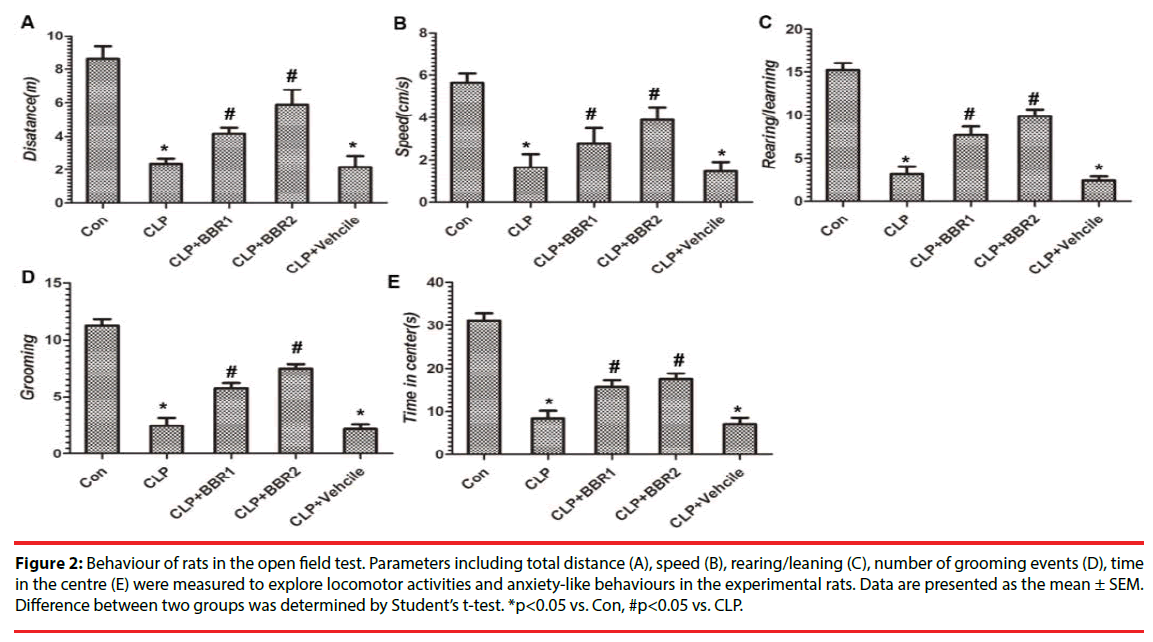
▪ Open field test
An open field test was used to evaluate both locomotor activity and anxiety-like behaviour [17] 6 days after the surgical procedure in our experiment. In brief, rats were placed into the central square and left to explore the area around for 5 min. Activities and traces were recorded via a video system. Total distance (m), speed (cm/s), frequency ratio of rearing/leaning, grooming activity, time in the centre (s) were all analysed afterwards.
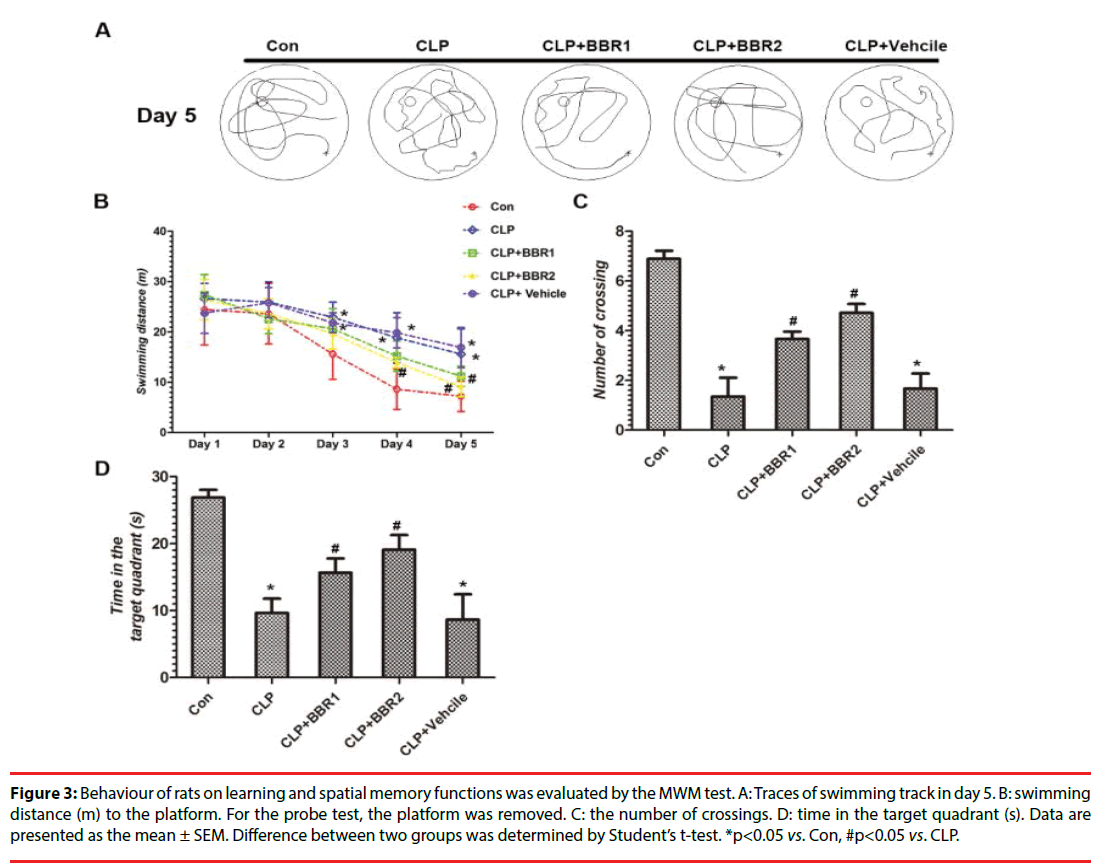
▪ Morris water maze test
The learning and memory deficits induced by numerous neurological diseases are often examined by the Morris water maze test, especially spatial memory dysfunction caused by damage to the hippocampus in the brain [18]. The Morris water maze test was conducted in a circular tank of 1.5 m diameter with a constant platform (5 cm diameter) that was beneath the surface of the water. Starting on day 10 after CLP surgery, each rat was trained for 4 consecutive days (4 trials per day) to find the submerged platform in 120 s. If the rat failed to find the platform in 120 s, it was gently guided to the platform by the experimenter and stayed for 30 s. After the training days, the platform was removed and the trial was operated on five groups of rats in 60 s. The swimming traces were tracked by the SLY-MWM system v.2.1 software. Then, the number of crossings and the time spent in the target quadrant were both analysed.
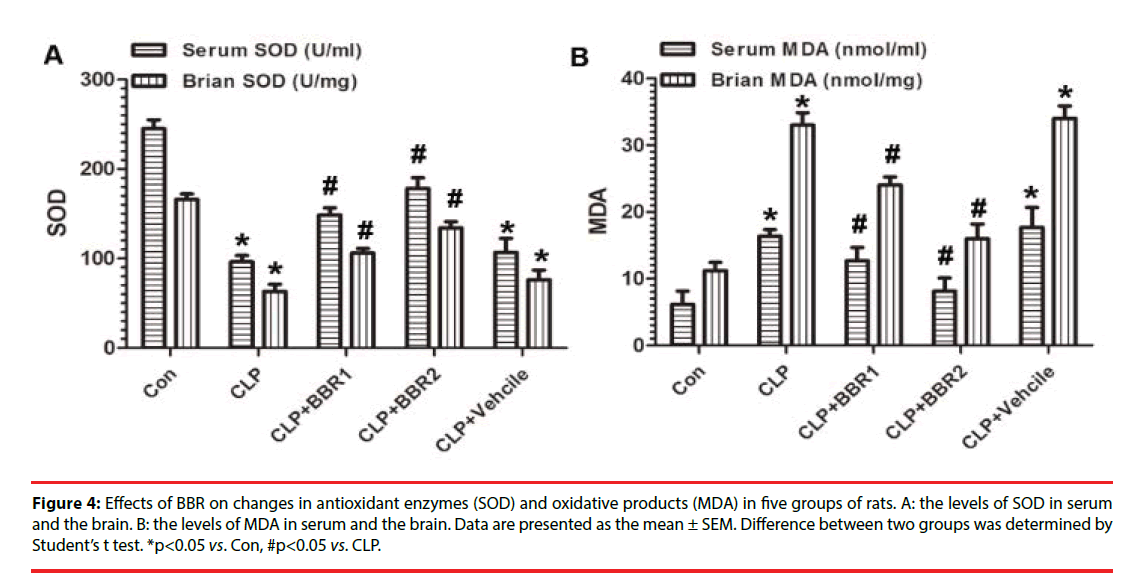
▪ Determination of oxidative stress parameters
The serum and brain tissues of half the number of experimental rats were extracted and homogenized immediately after the behaviour test. According to the instruction of the manufacture, SOD activity was measured spectrophotometrically by an SOD assay kit (Cayman Chemicals Co., Ann Arbor, Michigan, USA) at 440 nm. As an indicator of lipid peroxidation, the level of MDA was evaluated spectrophotometrically via measuring thiobarbituric acid reactive substances [19] in serum and brain tissue. The results were shown as U/ml in serum and U/mg in brain tissue.
▪ Determination of cytokines by ELISA and Western blotting assay
The levels of the cytokines IL-1β, IL-4, IL-6, and TNF-α in the brain tissue were all measured by a specific enzyme-linked immunosorbent assay (ELISA kits, R&D System, Minneapolis, MN, USA) according to the instructions of the manufacturer. The results of samples were analysed by microplate reader (Synergy TM H1, Bio Tek Instruments, Inc).
Western blot assay was also used to determine the levels of inflammatory cytokines in the brain tissue. Equal amounts of protein were resolved by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and transferred to PVDF membranes. After blocking with 5% BSA in 0.1% Tween 20 containing TBS, membranes were incubated with corresponding primary antibodies against IL-1β, IL-4, IL-6, TNF-α (Cell Signaling Technology, Boston, USA, dilutions at 1:1000) followed by incubation with horseradish peroxidase (HRP) labelled secondary antibodies for 1 h. Following washed by TBST 5 min × 3 times, the bands in membranes were visualized by ECL kit. The final results were analysed by ImageJ software.
▪ TUNEL and Immunohistochemistry (IHC) staining
Following perfusion and post-fixed with 4% paraformaldehyde, the brains of residual rats in five groups were removed to a 10%, 20%, or 30% sucrose solution for dehydration. Frozen coronal sections (20 μm) were obtained using a cryostat (Leica Microsystems, Germany). After extensive washing with PBS (5 min ×3 times), the sections were stained with a TUNEL kit (Roche Diagnostics, Indianapolis, IN) according to the standard protocol. After the TUNEL assay, anti-NeuN primary antibodies (Abcam, 1:500) and Alexa Fluor 488 secondary antibodies were used to stain brain sections in order to label the neurons. Finally, DAPI (Abcam, 1:500) was used to label the whole nucleus in the brain sections in 5 minutes. The apoptosis rate in the cerebral cortex region was calculated as the results. Briefly, twenty randomly fields were chosen to examine apoptotic cells in the cerebral cortex for each tissue specimen. The apoptotic rate was calculated as the ratio of apoptotic cells (Tunel-positive or red nuclei) to total cells (DAPI-positive or blue nuclei, ×100 to be expressed in percentage). The mean value was used for analysis.
▪ Histologic evaluation
The brain sections were routinely stained with haematoxylin and eosin. After extensive washing with PBS (5min ×3 times), the sections (especially hippocampus CA1 region) were observed under a light microscope.
Statistical Analysis
All experimental data were expressed as the mean ± SEM. The statistical comparison between two groups was carried out using Student’s t-test by Graphpad Prism 5 software. The value of p<0.05 was considered statistically significant.
Results
▪ BBR reduced mortality of rats after CLP
To evaluate the effect of BBR on sepsis rats, survival rate was first detected in different treatment groups. As seen from the Figure 1, the 6th day survival rates in the Con group was 100%. Conversely, rats in the CLP group showed a significant decreased survival rates in days 1, 2, and 3 compared with the Con group. Rats in the BBR1 and BBR2 treatment groups showed a higher survival rate compared with the CLP group, in which the protective effect was shown in a dose dependent manner. Whereas CLP treatment with vehicle resulted in similar survival rates versus the CLP group. This result showed that BBR partially abrogated the decrease in the survival rate induced by CLP surgery.
▪ BBR partially reversed the decreased locomotor activity and anxiety-like behaviour induced by CLP
In the open field test, the parameters containing total distance (m, Figure 2A), speed (cm/s, Figure 2B), rearing/leaning (Figure 2C), number of grooming events (Figure 2D), and time in the centres (s, Figure 2E) were assessed in this study. As we expected, CLP procedure significantly decreased the total distance, speed, rearing/leaning, number of grooming events, and time in the centers in contrast to Con group (p<0.05). BBR1 and BBR2 treatment groups partially reversed this reduction in motor total distance, speed, rearing/leaning, number of grooming, time in the centres caused by the CLP procedure. This partial improvement was observed to occur in a dose-dependent manner; that is, higher degrees were exhibited in the BBR2 group than in the BBR1 group. There was a significant reduction in the above parameters in the vehicle treatment group (p<0.05), which showed similar changes with the CLP group. Thereafter, we conclude that BBR improves the locomotor deficits and anxietylike behaviour induced by CLP procedure.
Figure 2: Behaviour of rats in the open field test. Parameters including total distance (A), speed (B), rearing/leaning (C), number of grooming events (D), time in the centre (E) were measured to explore locomotor activities and anxiety-like behaviours in the experimental rats. Data are presented as the mean ± SEM. Difference between two groups was determined by Student’s t-test. *p<0.05 vs. Con, #p<0.05 vs. CLP.
▪ Application of BBR improves learning and memory disorders after CLP surgery
Morris water maze test was applied to evaluate learning and memory disorders in experimental rats (Figure 3A). As is depicted in the Figure 3B, CLP rats swam significant longer distances to find the submerged platform at trial day 3 and day 4 (p<0.05). On experimental day 5, similar results were also shown between the Con and CLP groups (p<0.05). This result indicates that CLP induces learning disorders compared with Con rats. Treatment with BBR1 decreased the swimming distance in day 5 and BBR2 in day 4, day 5 versus CLP group (p<0.05) which demonstrates a protective effect of BBR in improving a learning disorder after CLP surgery. Treatment with the vehicle resulted in similar swimming distances as observed for the CLP group, which was significantly longer versus Con group (p<0.05). On experimental day 5, the number of crossings (Figure 3C) and time spent in the target quadrant (Figure 3D) were analysed to detect memory functions after CLP procedure. As is shown in the Figure 3C and 3D, the number of crossings and time spent in the target quadrant both decreased significantly in the CLP group versus Con group (p<0.05). Treatment with BBR1 and BBR2 partially reversed this decreasing trend in a dosedependent manner compared with the CLP group (p<0.05). The vehicle group exhibited similar changes as the CLP group. This result indicated that BBR treatment partially improved memory dysfunctions caused by CLP procedure. Overall, BBR improves learning and memory deficits induced by CLP procedure.
Figure 3: Behaviour of rats on learning and spatial memory functions was evaluated by the MWM test. A: Traces of swimming track in day 5. B: swimming distance (m) to the platform. For the probe test, the platform was removed. C: the number of crossings. D: time in the target quadrant (s). Data are presented as the mean ± SEM. Difference between two groups was determined by Student’s t-test. *p<0.05 vs. Con, #p<0.05 vs. CLP.
▪ BBR inhibited oxidative stress in serum and brain tissue
SOD and MDA levels for the serum and brain tissue are shown in the Figure 4. In the Figure 4A, the activities of the antioxidant enzymes SOD were markedly diminished in the CLP group both in the serum and brain tissue compared with Con group (p<0.05). Figure 4B shows that the levels of oxidative products MDA increased robustly not only in the serum but also in the brain tissue in CLP group versus Con group (p<0.05). BBR treatment significantly reversed the increasing effect of MDA and decreasing activities of SOD induced by CLP procedure in a dose-dependent manner (p<0.05). Treatment with vehicle group showed similar changes with CLP group, which exhibited higher levels of MDA and lower activities of SOD both in the serum and brain tissue versus Con group (p<0.05). This result indicates that BBR inhibits oxidative stress not only in serum but also in brain tissue.
Figure 4: Effects of BBR on changes in antioxidant enzymes (SOD) and oxidative products (MDA) in five groups of rats. A: the levels of SOD in serum and the brain. B: the levels of MDA in serum and the brain. Data are presented as the mean ± SEM. Difference between two groups was determined by Student’s t test. *p<0.05 vs. Con, #p<0.05 vs. CLP
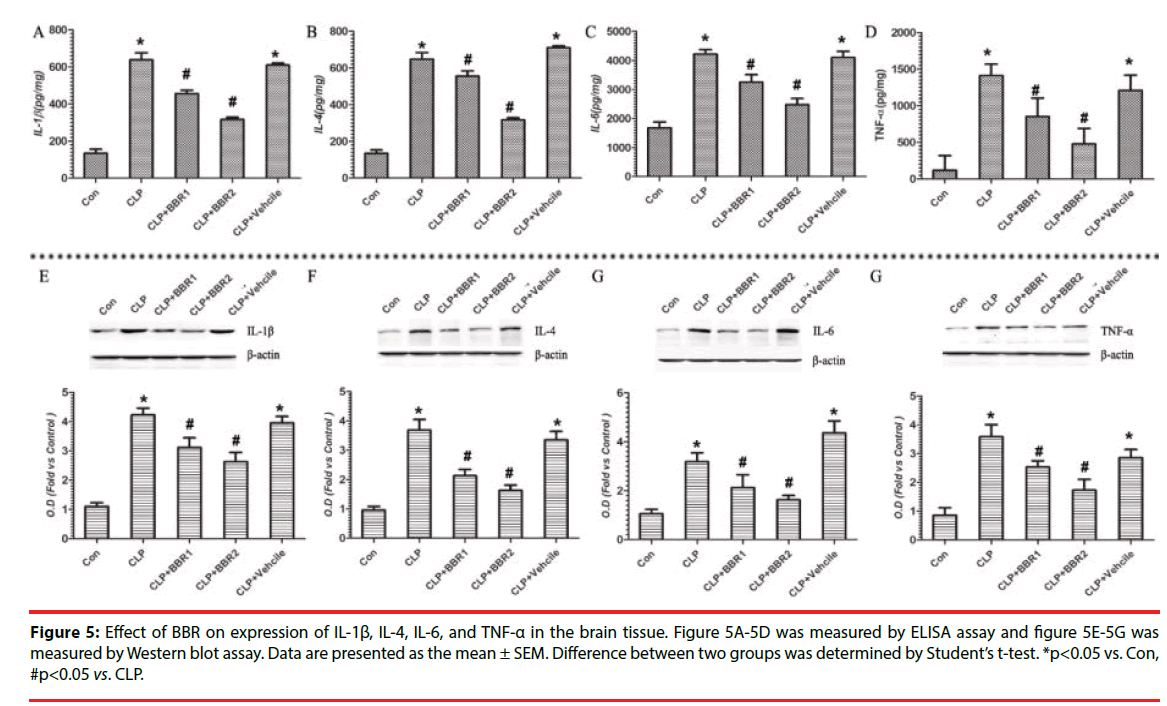
▪ BBR negatively regulates the levels of inflammatory cytokines in brain tissue
To determine the inflammation severity in the brain tissue, pro-inflammatory cytokines (IL-1β, IL-4, IL-6, TNF-α) were measured by ELISA (Figure 5A-5D) and Western blot assay (Figure 5E-5G). In the CLP group, the levels of inflammatory cytokines (IL-1β, IL-4, IL- 6, TNF-α) were significantly increased when compared with Con group (p<0.05). With BBR1 and BBR2 intervention, the cytokines levels were markedly reduced compared with CLP group (p<0.05) in a dose-dependent manner. Vehicle treatment significantly increased the levels of cytokines versus the Con group in this result (p<0.05). This result indicates that application of BBR inhibits the levels of inflammatory cytokines in the brain tissue.
Figure 5: Effect of BBR on expression of IL-1ß, IL-4, IL-6, and TNF-a in the brain tissue. Figure 5A-5D was measured by ELISA assay and figure 5E-5G was measured by Western blot assay. Data are presented as the mean ± SEM. Difference between two groups was determined by Student’s t-test. *p<0.05 vs. Con, #p<0.05 vs. CLP.
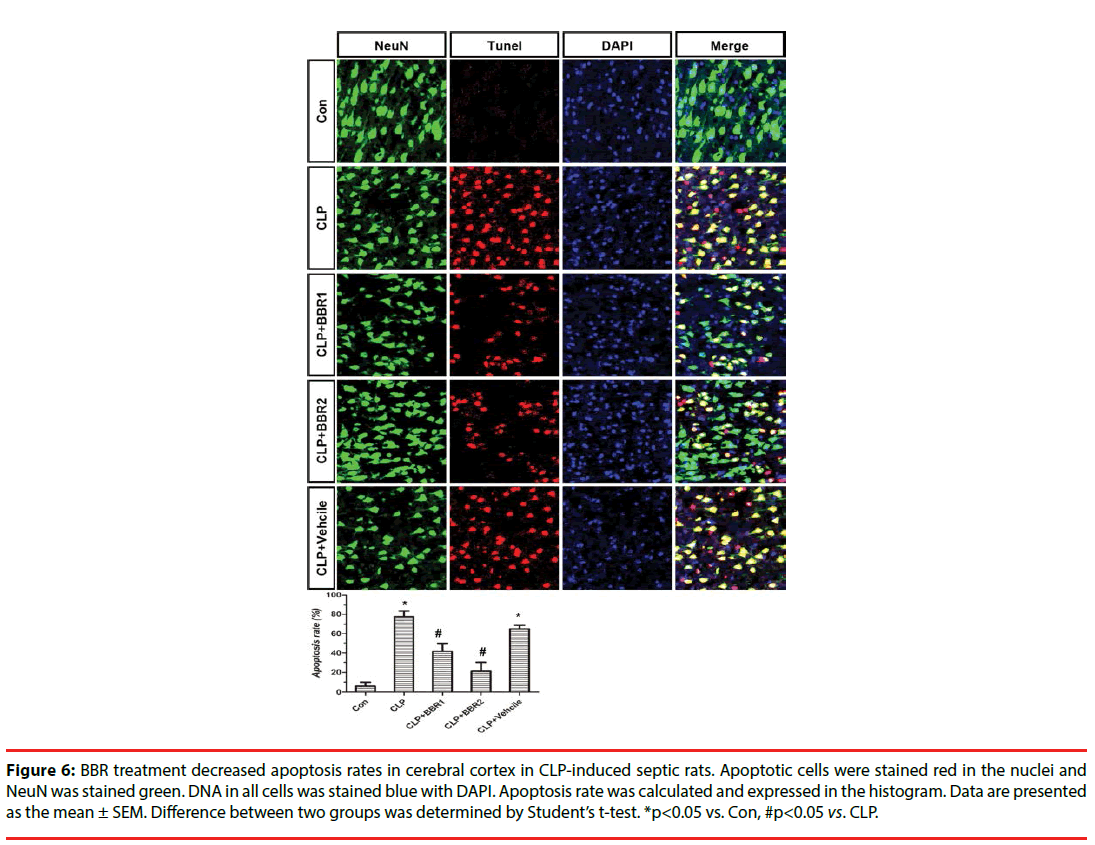
▪ BBR partially attenuated the apoptosis rates in cerebral cortex region
As depicted in the Figure 6, CLP surgery decreased the NeuN-positive and DAPI-positive signals in cerebral cortex regions compared with Con rats. Treatment with BBR partially reversed the cell loss versus CLP treatment group in a dose-dependent manner.
Figure 6: BBR treatment decreased apoptosis rates in cerebral cortex in CLP-induced septic rats. Apoptotic cells were stained red in the nuclei and NeuN was stained green. DNA in all cells was stained blue with DAPI. Apoptosis rate was calculated and expressed in the histogram. Data are presented as the mean ± SEM. Difference between two groups was determined by Student’s t-test. *p<0.05 vs. Con, #p<0.05 vs. CLP.
The effect of BBR on apoptotic cells in cerebral cortex region of septic rats was investigated by Tunel staining. As is shown in the Figure 6, there was no Tunel-positive signals in the cerebral cortex region of Con rats. Conversely, the apoptosis rate exhibited in the the cerebral cortex region of CLP group was increased significantly versus the Con group (p<0.05). Interventions with BBR attenuated the higher apoptosis rate caused by CLP surgery only (p<0.05) in a dose dependent manner. Treatment with vehicle also caused higher apoptosis rate compared with Con group (p<0.05). This picture we observed by Tunel staining showed that BBR prevented apoptosis rate in the cerebral cortex region of CLPinduced septic rats.
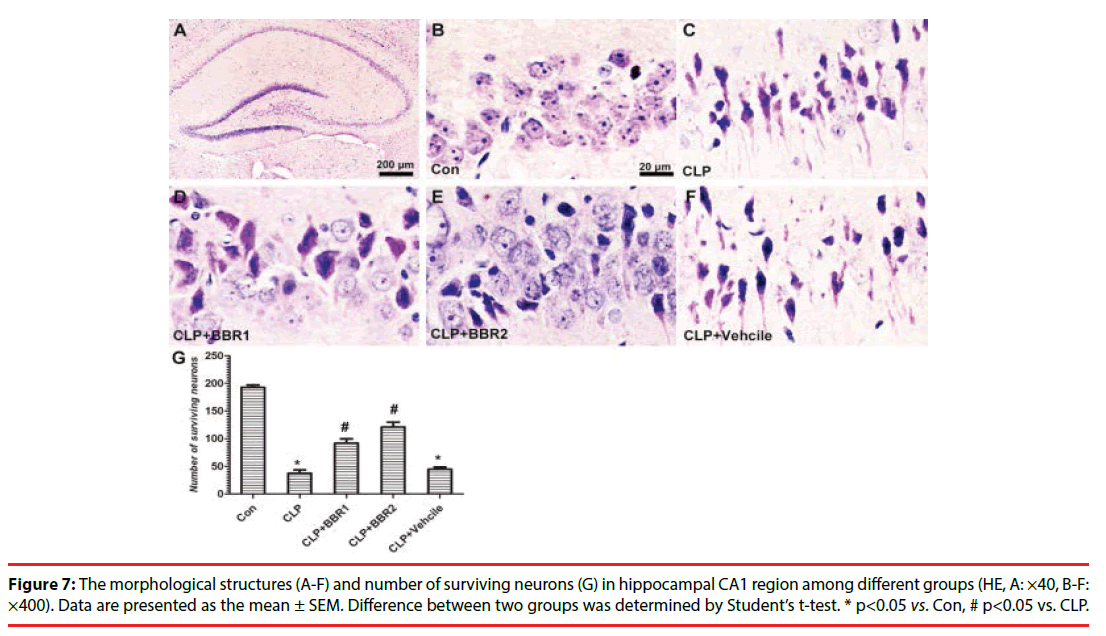
▪ Histological changes in hippocampus CA1 region
HE staining was used to detect the histological changes induced by CLP procedure in the hippocampus CA1 region (Figure 7A). As is depicted in the Figure 7B, normal neuronal density and cell morphology were well preserved in the Con group. Conversely, hippocampal cells were arranged in disorder. The structure of neurons appeared nuclear pyknosis, karyorrhexis and vacuolation which phenomenon presents acute traumatic changes (Figure 7C). In BBR1 and BBR2 treated groups, the aforementioned abnormal changes of neurons were partially lessened after CLP injury (Figure 7D, 7E). The vehicle-treated group showed similar morphological changes with CLP group (Figure 7F). The number of surviving neurons was calculated, as shown in the Figure 7G, CLP procedure induced significant death of neurons in hippocampal CA1 regions compared with Con group (p<0.05). Administration with BBR partially rescued the neuron loss caused by CLP in dose dependent manner (p<0.05). The vehicle-treated group showed similar number of survival neurons in the CA1 region. This result revealed that BBR could protect neurons in CA1 region from apoptosis induced by CLP.
Discussion
In terms of morbidity and mortality among various serious diseases, sepsis imposes a substantial global burden and needs to be diagnosed and treated as soon as possible [20]. Previous reports also revealed that BBR and its derivatives have broadly anti-inflammatory and anti-tumour effects and could act as a novel drug towards diseases [21]. In this study, we demonstrated that the application of BBR before the induction of sepsis was able to prevent the development of cognitive dysfunction in rats surviving from faecal peritonitis. Further research revealed that this protective effect towards cognitive disorder was tightly related to the reduction of pro-inflammatory cytokines, the onset of oxidative damage and the prevention of apoptosis in neurons in the hippocampal CA1 region.
Excessive inflammation and oxidative stress were recognized as the underlying mechanism in cognitive impairments caused by sepsis [22,23]. After that, severe acute kidney injury [24,25], lung injury [26], liver failure [27] as well as cognitive impairments were all detrimental to sepsis patients. Early research reported that BBR combination with yohimbine was helpful in the early phase of sepsis in which drugs were administered 2 h after CLP surgery [15]. Combined with our research, BBR administration alone before CLP surgery also showed beneficial effects towards sepsis in animals. Further mechanisms underlying these anti-inflammatory and antioxidative effects of BBR were still unknown. Many signalling pathways, including CCR2 expression in neutrophils [15], Toll-like receptors [14], NF-ΚB [28], and PPARγ [29], were targets of BBR in vitro or vivo. In addition, some effects of BBR were significantly enhanced by combination with Yohimbine treatment [30]. Whether BBR combination treatment with Yohimbine before CLP surgery will show an increasing beneficial effect towards sepsis induced cognitive impairment and precise mechanisms underlying this effect still remain to be further explored.
Results
Our results proved that pretreatment with BBR improved the survival rate and cognitive impairment via inhibiting the levels of cytokines, oxidative stress and apoptosis in neurons in the brain after sepsis, which means BBR is a potential promising drug in treating sepsis disease in the near future in patients. Conversely, there are some gaps existing between rats and human studies. In preclinical mouse studies, more than a hundred promising therapies were developed to prevent inflammatory responses via activating immunosuppressive pathways to improve survival rates. It’s a pity that these therapies universally failed to exhibit efficacy in human patients with sepsis [31-34]. Though murine models help us to better understand the pathophysiological changes of disease and drugs, there is also some limitations existing between murine and human patients, including differences in interspecies, strains, environments, innate immunity and adaptive immunity [33]. Whereas in clinical research, BBR acts as a nonprescription drug with confirmed safety to treat diarrhoea and gastrointestinal disorders. Many berberine derivative compounds were synthesized and evaluated bioactivity in treating various diseases [35,36]. Whether BBR and its derivatives treatment before the formation of sepsis shows efficacy in avoiding cognitive dysfunction after sepsis patients in clinical research is still unknown and needs to be further studied. Whether BBR also failed in clinical research towards sepsis patients or not, BBR is one of the effective promising drugs in avoiding the establishment of cognitive dysfunction in a pathophysiology study in rats and some research towards the inherent differences between septic rodents and human sepsis patients who need to be explored in the near future.
Conclusion
Overall, our research provides new promising drugs in avoiding the establishment of cognitive disorders induced by sepsis – BBR. Through its anti-inflammatory, antioxidative and inhibition of neuronal apoptosis occurrence in the hippocampal CA1 region, BBR significantly improved the survival rates and cognitive functions in septic rats. Therefore, BBR is a potential drug of septic rats in which efficacy in human patients needs to be further explored.
Conflict of Interest Statement
The authors declare no competing financial interests.
Acknowledgements
This work was supported by the Jiangsu Province Natural Science Foundation of China (BK20151204).
References
- Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315(8), 801-810 (2016).
- Bleck TP, Smith MC, Pierre-Louis SJ, et al. Neurologic complications of critical medical illnesses. Crit. Care. Med 21(1), 98-103 (1993).
- Eidelman LA, Putterman D, Putterman C, et al. The spectrum of septic encephalopathy. Definitions, etiologies, and mortalities. JAMA 275(6), 470-473 (1996).
- Scragg P, Jones A, Fauvel N. Psychological problems following ICU treatment. Anaesthesia 56(1), 9-14 (2001).
- Chaudhry N, Duggal AK. Sepsis Associated Encephalopathy. Adv. Med 762320 (2014).
- Vincent JL, Opal SM, Marshall JC, et al. Sepsis definitions: time for change. Lancet 381(9868), 774-775 (2013).
- Ledderose C, Bao Y, Kondo Y, et al. Purinergic Signaling and the Immune Response in Sepsis: A Review. Clin. Ther 38(5), 1054-1065 (2016).
- Hotchkiss RS, Karl IE. The pathophysiology and treatment of sepsis. N. Engl. J. Med 348(2), 138-150 (2003).
- Salvemini D, Cuzzocrea S. Oxidative stress in septic shock and disseminated intravascular coagulation. Free. Radic. Biol. Med 33(9), 1173-1185 (2002).
- Hara N, Chijiiwa M, Yara M, et al. Metabolomic Analyses of Brain Tissue in Sepsis Induced by Cecal Ligation Reveal Specific Redox Alterations--Protective Effects of the Oxygen Radical Scavenger Edaravone. Shock 44(6), 578-584 (2015).
- Zhong W, Qian K, Xiong J, et al. Curcumin alleviates lipopolysaccharide induced sepsis and liver failure by suppression of oxidative stress-related inflammation via PI3K/AKT and NF-kappaB related signaling. Biomed. Pharmacother 83(1), 302-313 (2016).
- Li Y, Wang F, Luo Y. Ginsenoside Rg1 protects against sepsis-associated encephalopathy through beclin 1-independent autophagy in mice. J. Surg. Res 207(1), 181-189 (2017).
- Wang K, Feng X, Chai L, et al. The metabolism of berberine and its contribution to the pharmacological effects. Drug. Metab. Rev 49(2), 139-157 (2017b).
- Li GX, Wang XM, Jiang T, et al. Berberine Prevents Intestinal Mucosal Barrier Damage During Early Phase of Sepsis in Rat through the Toll-Like Receptors Signaling Pathway. Korean. J. Physiol. Pharmacol 19(1), 1-7 (2015).
- Wang Y, Wang F, Yang D, et al. Berberine in combination with yohimbine attenuates sepsis-induced neutrophil tissue infiltration and multiorgan dysfunction partly via IL-10-mediated inhibition of CCR2 expression in neutrophils. Int. Immunopharmacol 35(), 217-225 (2016).
- Otero-Anton E, Gonzalez-Quintela A, Lopez-Soto A, et al. Cecal ligation and puncture as a model of sepsis in the rat: influence of the puncture size on mortality, bacteremia, endotoxemia and tumor necrosis factor alpha levels. Eur. Surg. Res 33(2), 77-79 (2001).
- Walsh RN, Cummins RA. The Open-Field Test: a critical review. Psychol. Bull 83(3), 482-504 (1976).
- Morris RG, Garrud P, Rawlins JN, et al. Place navigation impaired in rats with hippocampal lesions. Nature 297(5868), 681-683 (1982).
- Mihara M, Uchiyama M. Determination of malonaldehyde precursor in tissues by thiobarbituric acid test. Anal. Biochem 86(1), 271-278 (1978).
- van der Poll T, van de Veerdonk FL, Scicluna BP, et al. The immunopathology of sepsis and potential therapeutic targets. Nat. Rev. Immunol 17(7), 407-420 (2017)
- Zou K, Li Z, Zhang Y, et al. Advances in the study of berberine and its derivatives: a focus on anti-inflammatory and anti-tumor effects in the digestive system. Acta. Pharmacol. Sin 38(2), 157-167 (2017).
- Moraes CA, Santos G, de Sampaio e Spohr TC, et al. Activated Microglia-Induced Deficits in Excitatory Synapses Through IL-1beta: Implications for Cognitive Impairment in Sepsis. Mol. Neurobiol 52(1), 653-663 (2015).
- Schwalm MT, Pasquali M, Miguel SP, et al. Acute brain inflammation and oxidative damage are related to long-term cognitive deficits and markers of neurodegeneration in sepsis-survivor rats. Mol. Neurobiol 49(1), 380-385 (2014).
- Fisher J, Russell JA, Bentzer P, et al. Heparin-Binding Protein (HBP): A Causative Marker and Potential Target for Heparin Treatment of Human Sepsis-Induced Acute Kidney Injury. Shock 48(3), 313-320 (2017).
- Wang N, Mao L, Yang L, et al. Resveratrol protects against early polymicrobial sepsis-induced acute kidney injury through inhibiting endoplasmic reticulum stress-activated NF-kappaB pathway. Oncotarget 8(22), 36449-36461 (2017c).
- Hansen LW, Yang WL, Bolognese AC, et al. Treatment with milk fat globule epidermal growth factor-factor 8 (MFG-E8) reduces inflammation and lung injury in neonatal sepsis. Surgery 162(2), 349-357 (2017).
- Wu T, Wang L, An J, et al. Noninvasive Imaging of Stored Red Blood Cell-Transfusion Aggravating Sepsis-Induced Liver Injury Associated with Increased Activation of M1-Polarized Kupffer Cells. Shock (2017).
- Wang YY, Li HM, Wang HD, et al. Pretreatment with berberine and yohimbine protects against LPS-induced myocardial dysfunction via inhibition of cardiac I-[kappa]B[alpha] phosphorylation and apoptosis in mice. Shock 35(3), 322-328 (2011).
- Feng AW, Gao W, Zhou GR, et al. Berberine ameliorates COX-2 expression in rat small intestinal mucosa partially through PPARgamma pathway during acute endotoxemia. Int. Immunopharmacol 12(1), 182-188 (2012).
- Li H, Wang Y, Zhang H, et al. Yohimbine enhances protection of berberine against LPS-induced mouse lethality through multiple mechanisms. PLoS. One 7(12), e52863 (2012).
- Dyson A, Singer M. Animal models of sepsis: why does preclinical efficacy fail to translate to the clinical setting? Crit. Care. Med 37(1Suppl), S30-S37 (2009).
- Fink MP. Animal models of sepsis. Virulence 5(1), 143-153 (2014).
- Stortz JA, Raymond SL, Mira JC, et al. Murine Models of Sepsis and Trauma: Can We Bridge the Gap? ILAR. J 1-16 (2017).
- Zanotti-Cavazzoni SL, Goldfarb RD. Animal models of sepsis. Crit. Care. Clin 25(4), 703-719 (2009).
- Wang J, Yang T, Chen H, et al. The synthesis and antistaphylococcal activity of 9, 13-disubstituted berberine derivatives. Eur. J. Med. Chem 127(), 424-433 (2017a).
- Xiao D, Liu Z, Zhang S, et al. Berberine Derivatives with Different Pharmacological Activities via Structural Modifications. Mini. Rev. Med. Chem (2017).