Review Article - (2018) Volume 8, Issue 3
Prevalence of Posttraumatic Stress Disorder in Schizophrenia Spectrum Disorders: A Systematic Review
- Corresponding Author:
- Eric Fakra
Department of Psychiatry, University Hospital of Saint-Etienne, Saint-Etienne, France; TAPE Laboratory, EA7423, Jean Monnet University, Saint-Etienne, France
Tel: 04 77 32 77 05
Abstract
Background
Posttraumatic stress disorder (PTSD) is a comorbidity often ignored and unexplored in patients with schizophrenia, despite a possible impact on its symptomology. Links and interactions between these disorders are still unknown. This article proposes a systematic review of the prevalence of PTSD in schizophrenia spectrum disorders (SSD).
Methods and findings
Thirty-eight studies were included.
Results
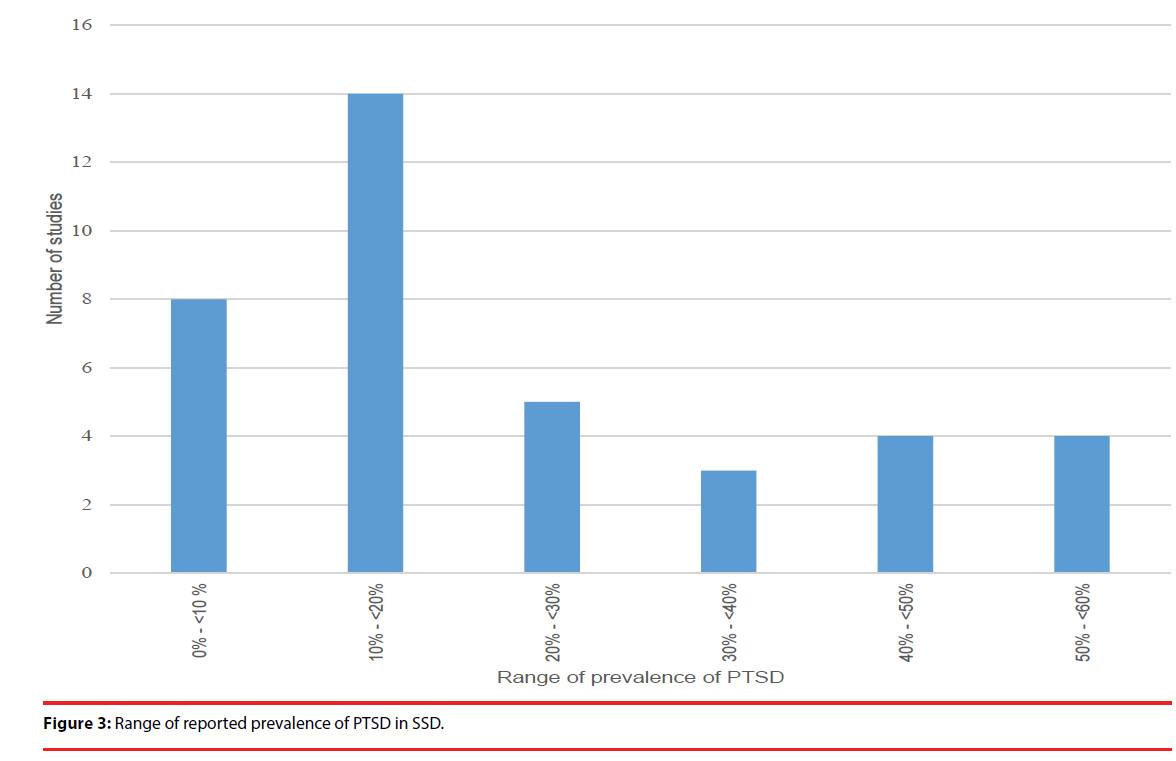
Results were heterogeneous with range of prevalence of PTSD varying between 0% and 55%. These wide ranges of prevalence were explained by the utilization of different assessment tools of trauma exposure, not all validated and heterogeneous population of SSD (schizoaffective disorders, comorbid addiction disorders mainly). Nevertheless, 78,9% of the studies found a prevalence of PTSD superior to 10 %.
Conclusion
Our review suggests a high rate of prevalence of PTSD in schizophrenia, which may be underestimated due to symptoms overlap. Moreover, the absence of difference in trauma exposure between SSD and the general population evokes an increased liability to trauma in patients with SSD.
Keywords
PTSD, Trauma, Schizophrenia, Schizoaffective, Prevalence, Posttraumatic
Introduction
Schizophrenia is a severe mental illness which has a considerable impact on quality of life. Its worldwide prevalence is estimated between 0,3 % and 0,7% [1]. The physio-pathology of schizophrenia is still unexplained. The first hypothesis was the dopaminergic hypothesis [2,3]. It suggests that there is a hyperactive dopamine transmission in the mesolimbic areas, responsible for positive symptoms in the disorder and a prefrontal dopaminergic hypoactive dopamine transmission in the prefrontal cortex responsible for negative symptoms and cognitive alterations. But this hypothesis could not explain all by itself the emergence of schizophrenia in patients and other neurotransmitters are suspected to be involved such serotonin and glutamate [4]. The now most prevalent hypothesis is the stress-vulnerability model [5]. Schizophrenia would be the results of associations between genetic factor [6,7] and environmental risks such as stress, in particular childhood trauma [8]. It was shown that a history of childhood trauma in patients with schizophrenia is associated with increased stress reactivity later in life, with more severe symptoms as well as lower quality of life [9-11]. Nevertheless, the role of adulthood trauma in schizophrenia is not well known. Over the last 20 years, there has been a growing literature on the subject, especially on posttraumatic stress disorder (PTSD) and schizophrenia. PTSD is defined by experiencing a traumatic event and characterized by a group of 3 main symptoms: flashbacks, withdrawal and hyper vigilance [12]. People with PTSD can also experience hallucinations, social isolation and dissociative symptoms [13] which can overlap with schizophrenia symptoms. PTSD is often underdiagnosed in general population [14,15] and largely underdiagnosed in people with schizophrenia [16], even if anxiety disorders are among the most frequent comorbidities of this disorder [17]. A meta-analysis recensing this comorbidity [18] found that 38,3% of patients with schizophrenia had an anxiety disorder with 12,4% had a comorbid PTSD. However, this meta-analysis does not specifically address the comorbidity between schizophrenia and PTSD. Moreover, several studies since this work have questioned the links between these two disorders.
Our objective was to conduct a systematic review of studies having assessed the prevalence of PTSD in schizophrenia spectrum disorders (SSD), including studies published before and after Achim et al. metaaalysis.
Methods
▪ Data search
A literature review was performed on MEDLINE. We included articles until 30 June 2017. Keywords were: PTSD or posttraumatic stress disorder and schizophrenia.
▪ Inclusion criteria
Prevalence of PTSD was the main inclusion criteria. Only articles with adult patients were included. Main diagnosis needed to be a schizophrenia spectrum disorder (SSD: schizophrenia, schizoaffective disorder or schizophreniform disorder). Studies about severe mental illnesses (bipolar disorder, schizophrenia, depression, anxiety disorders, personality disorders and eating behavior disorder) were included only if data was available for SSD. Exclusion criteria were a main diagnosis of mood disorder (depression or bipolar disorder) and underage populations.
▪ Selection
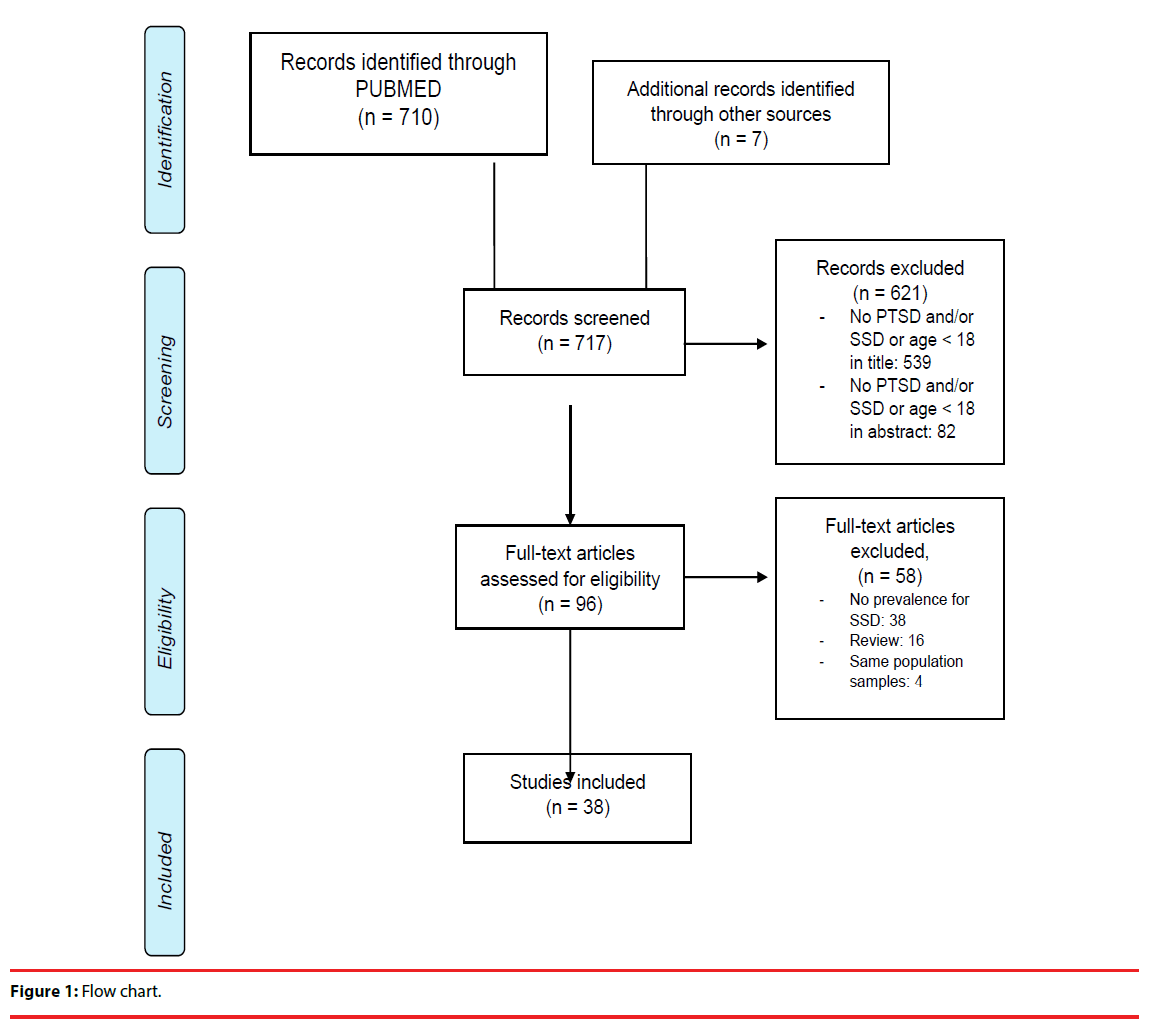
The selection of articles is detailed in Figure 1. We obtained 710 hits in PubMed, seven studies were found through reference lists of the articles we included. On 717 articles, 621 were excluded from title or abstract because they did not mention schizophrenia spectrum disorder and/ or trauma or PTSD or the population age was under 18 years old. From the 96 studies left for full text reading, 58 were excluded (38 did not mention a prevalence of PTSD, 16 were reviews and four used the same sample of patients as others included studies). 38 studies are included.
▪ Data extraction
The following data were extracted: demographics characteristics, sample size, instruments used to assess SSD, instruments used to assess PTSD, instruments used to assess trauma exposure, prevalence of PTSD, prevalence of trauma exposure (when available).
If there was a lifetime and a current value for prevalence of PTSD, only current value was included.
Flow chart is Figure 2.
▪ Data availability
All data analysed during this study are included in this published article.
Results
The contents of the articles are summed up in Table 1. Studies started from 1995 to 2016. Studies prior to 1995 didn’t have homogeneous population in terms of diagnosis (schizophrenia, delusional mania, acute psychotic episode) or a formal indication of diagnosis (patients labelled with psychosis without any specification, no validation with International Classification of Diseases or Diagnostic and Statistical Manual of Mental Disorders; DSM).
| Authors | Country | Population | Number of patients (% men) |
Mean age (SD) | Assessment | Prevalence of trauma exposure | Prevalence of PTSD | ||
|---|---|---|---|---|---|---|---|---|---|
| SSD | Trauma exposure | PTSD | |||||||
| Aakre et al. [1] | USA | Female drug addict outpatients | 42 (0%) | 41,0 (6,8) | SCID-4 | TLEQ | CAPS-S | 100% | 48% |
| Alvarez et al. [2] | Spain | Outpatients | 62 (64,5%) | 39,4 (10,4) | DSM-IV | TLEQ | DEQ | 88,2% | SCZ: 10,2% SZA: 22,2% |
| Birgenheir et al. [3] | USA | Outpatients | 87006 (93,3%) | - | Charts | - | Charts | - | 15,2 % |
| Braga et al. [4] | Brazil | Outpatients | 53 (71,7%) | - | DSM-IV | - | SCID-4 | - | 3,8% |
| Calhoun et al. [5] | USA | Veteran inpatients | 165 (100%) | 48 (7,8) | SCID-4 | SAEQ CTS CES |
PCL | 96% | 47% |
| Chapleau et al. [6] | USA | Inpatients and outpatient | 60 (93,3%) | 50,3 (11,09) | SCID-3 | - | PCL | - | 55% |
| Fan et al. [7] | USA | Outpatients | 87 (74,7%) | 43,7 (8,9) | SCID-4 | HTQ | HTQ | 100% | 17% |
| Frame and Morrison [8] | UK | Outpatients | 60 (61,7%) | - | DSM-IV | - | DTS | - | 50% |
| Gearon et al. [9] | USA | Female drug addict outpatients | 54 (0%) | 40,6 (6,8) | SCID-4 | TLEQ | CAPS-S | 96% | 46% |
| Halasz et al. [10] | Hungary | Outpatients | 125 (55,2%) | - | SCID-4 | - | CAPS | - | 17% |
| Harvey et al. [11] | USA | Outpatients | 3445 (93%) | 55,3 (9,9) | DSM-IV | - | MINI | - | 22% |
| Kennedy et al. [12] | USA | Outpatients | 30 (-) | - | DSM-IV | - | Penn PTSD | - | 23,3% |
| Kilcommons and Morrison [13] | UK | Outpatients | 32 (78,1%) | 34,5 (9,96) | DSM-IV | THQ | PSS | 94% | 53,1% |
| Lommen and Restifo [14] | Netherlands | Outpatients | 33 (69,7%) | 42,3 (10,6) | Charts | THQ | PSS | 97% | 9,1% |
| Lyon et al. [15] | USA | Twin outpatients | 24 (100%) | 44,6 | Charts | - | DIS-III-R | - | 16,7% |
| Meyer et al. [16] | Finland | Inpatients and outpatients | 46 (39%) | 40,8 (12,1) | DSM-IV | - | CAPS | - | 11% |
| Mueser et al. [17] | USA | Inpatients and outpatients | 94 | - | DSM-IV Charts SCID-4 |
THQ | PCL | 98% | 30,9% |
| Mueser et al. [18] | USA | Inpatients and outpatients | 526 | - | SCID-4 | - | PCL | - | 31,6% |
| Nebioglu and Altindag [19] | Turkey | Outpatients | 82 (76,8%) | - | DSM-IV | - | SCID-4 | - | 7,3% |
| Neria et al. [20] | USA | Outpatients | 165 (-) | - | DSM-IV | DIS-3-R | DIS-III-R | 68,5% | 10% |
| Newman et al. [21] | USA | Inpatients | 70 (71,4%) | - | DSM-IV | SLESQ | SCID-4 | 12,8% | 87% |
| Ng et al. [22] | USA | Outpatients | 125 (75,2%) | 44,05 (9,51) | DSM-IV | HTQ | HTQ | 12% | 82% |
| Pallanti et al. [23] | Italy | Outpatients | 80 (48,8) | 29 (5,9) | SCID-4 | - | SCID4 | - | 1,3% |
| Peleikis et al. [24] | Norway | Inpatients and outpatients | 292 (55,1%) | - | SCID-4 | MINI | MINI | 25% | 7% |
| Picken and Tarrier [25] | UK | Drug addict outpatients | 110 (90%) | 37 (9,95) | SCID-4 | PDS | PDS CAPS-S |
91% | 9% |
| Pollice et al. [26] | Italy | Inpatients | 54 (69,2%) | 44,6 (14,1) | SCID-4 | - | IES SCDI-4 |
100% | 17% |
| Priebe et al. [27] | Germany | Outpatients | 105 (44,8%) | 38,6 (9,4) | DSM-III | - | PTSD-I | - | 51% |
| Renard et al. [28] | USA | Veteran outpatients |
49 (91,8%) | 51,8 (9,8) | SCID-4 | - | PCL | - | 43% |
| Resnick et al. [29] | USA | Outpatients | 47 (36,2%) | 44,1 (9,7) | SCID-4 | THQ | CAPS | 97,9% | 12,8% |
| Rosenberg et al. [30] | USA | Outpatients | 569 (67,8%) | 42 (9) | SCID-4 | - | PCL | - | 34% |
| Schäfer et al. [31] | Germany | Inpatients | 145 (66,9%) | 34,1 | SCID-4 | STI | SCID4 | - | 12% |
| Seedat et al. [32] | South Africa | Inpatients | 70 (54,3%) | 35,8 (11,2) | Charts MINI |
- | MINI | - | 4,3% |
| Sin et al. [33] | Singapore | Inpatients and outpatients | 45 (-) | SCID-4 | - | CAPS | - | 15,5% | |
| Steinert et al. [34] | Germany | Inpatients | 118 (47,5%) | - | ICD-10 | DSM-IV A criteria |
SCID4 PDS |
49,2% | 28% |
| Strakowski et al. [35] | USA | Outpatients | 18 (50%) | 37,2 (20,5) | SCID-3 | - | SCID3 | - | 22% |
| Strauss et al. [36] | USA | Outpatients | 70 (57,1%) | 42,4 (-) | SCID-4 | - | CAPS | - | 21,4% |
| Tibbo et al. [37] | Canada | Outpatients | 32 (78%) | - | MINI | - | MINI CAPS |
- | 0% |
| Vogel et al. [38] | Germany | Inpatients | 74 (66,2%) | 39 (14) | DSM-IV | - | DSM-III | - | 15,5% |
CTS: Conflict Tactics Scale PSS-I: PTSD Symptom Scale - Interview
DEQ: Distressing Events Questionnaire PTSD-I: PTSD-Interview
DIS-III-R: Diagnostic Interview Schedule SAEQ: Sexual Abuse Exposure Questionnaire
DTS: Davidson Trauma Scale SCZ: schizophrenia
HTQ: Harvard Trauma Questionnaire SLESQ: Stressful Life Events Screening Questionnaire
IES: Impact of Event Scale STI: Structured Trauma Interview
MINI: Mini International Neuropsychiatric Interview SZA: schizoaffective disorder
Table 1: Studies results.
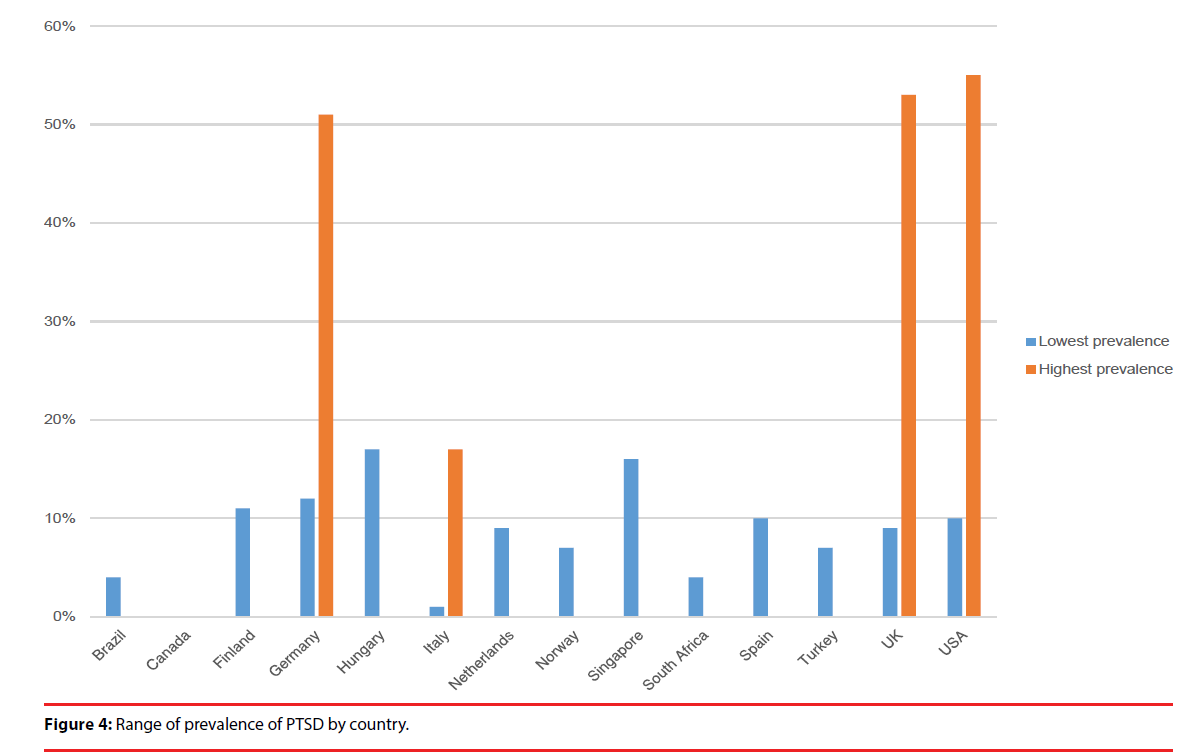
▪ Countries
On 38 studies, 55,2 % took place in America and 37% in Europe. Countries which most investigated PTSD in SSD were USA (n=19), Germany (n=4) and UK (n=3). Other studies were conducted in Asia (n=2) and Africa (n=1).
▪ Sample characteristics
Twenty-one studies included outpatients, nine included inpatients and five included both inpatients and outpatients. One study used registries and two studies did not specify the kind of sample. Eleven studies included only patients with a schizophrenia diagnosis and excluded patients with schizoaffective disorder. Sample size varies from 18 to 87006 patients. Thirteen studies included more than 100 patients. Three studies included only SSD with substance use disorder. Two included only men and two only women. Mean age was between 29 years old (SD=5,9) and 55,3 years old (SD=9,9).
▪ Diagnostic tools for SSD
Most studies used DSM-IV for establishing SSD diagnosis, three used DSM-III and none used DSM5. 50 % used Structured Clinical Interview for DSM (SCID), three used charts to confirm SSD diagnosis.
▪ Assessment of trauma exposure
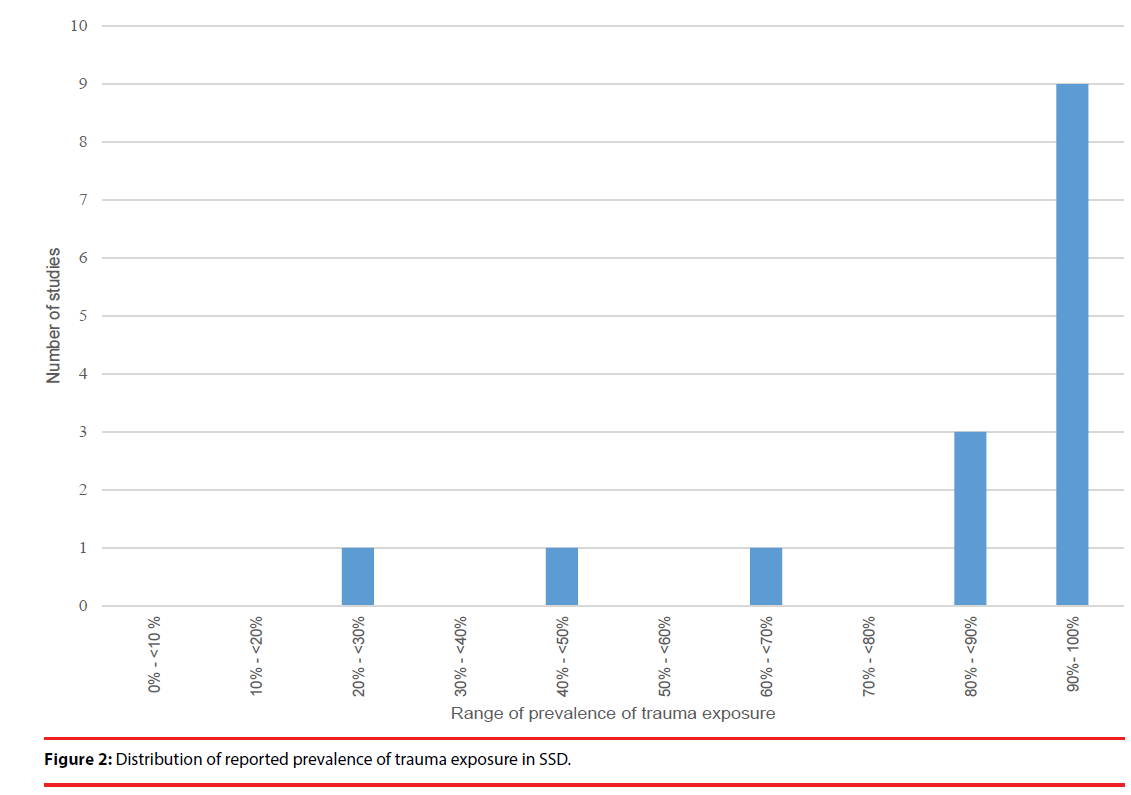
Not all studies investigate trauma exposure. Only 15 studies reported the prevalence of trauma exposure. The two most used tools for assessing trauma exposure were Trauma History Questionnaire (THQ; n=4) and Traumatic Life Events Questionnaire (TLEQ ; n=3).
▪ Prevalence of trauma exposure
Range of prevalence of trauma exposure starts from 25 to 100 % (Figure 3). Two studies were excluded because trauma exposure was one of the inclusion criteria [19,20]. 12 of the 15 studies find a trauma exposure superior to 80%.
▪ Assessment of PTSD
There is an important heterogeneity in assessment tools for prevalence of PTSD in the included studies (Table 2). Fifteen different methods were used. Twenty-three studies used an interview tool, 11 used a self-report tool and three combined an interview tool and a selfreport tool. One study was based on registries. The three most used assessment tools were the Clinician Administered PTSD Scale (CAPS ; n= 9 including CAPS-S n=3), the SCID (n=8) and the Posttraumatic Stress Disorder CheckList (PCL ; n=6). Among tools designed specifically for PTSD screening and diagnosis, only the CAPS-S and the PCL have a validity study in patients with SSD.
| Screening tools | Interview or self-report | Validation study in general population | Validation study in SSD | Number of studies | Studies |
|---|---|---|---|---|---|
| CAPS | Interview | Blake et al. [39] | CAPS-S: Gearon et al. [40] | 9 3 CAPS-S | CAPS: Halasz et al. [10] Meyer et al. [16] Resnick et al. [29] Sin et al. [33] Strauss et al. [36] Tibbo et al. [37] CAPS-S: Aakre et al. [1] Gearon et al. [9] Picken and Tarrier [25] |
| DEQ | Self-report | Kubany et al. [41] | - | 1 | Alvarez et al. [2] |
| DIS-III-R | Interview | Robins et al. [42] | Robins et al. [42] | 2 | Lyons et al. Neria et al. [20] |
| DTS | Self-report | Davidson et al. [43] | - | 1 | Frame and Morrison [8] |
| HTQ | Self-report | Mollica et al. [44] | - | 2 | Fan et al. [7] Ng et al. [22] |
| IES | Self-report | Zilberg et al. [45] | - | 1 | Pollice et al. [26] |
| SCID | Interview | DSM-III: Spitzer et al. [46] DSM-IV: First et al. [47] |
DSM-III: Spitzer et al. [46] DSM-IV: First et al. [47] |
8 | Braga et al. [4] Nebioglu and Altindag [19] Newman et al. [21] Pallanti et al. [23] Pollice et al. [26] Schäfer et al. [31] Steinert et al. [34] Strakowski et al. [35] |
| MINI | Interview | Sheehan et al. [48] | Sheehan et al. [48] | 4 | Harvey et al. [11] Peleikis et al. [24] Seedat et al. [32] Tibbo et al. [37] |
| PCL-S | Self-report | Weathers et al. [49] | PCL-5: Steel et al. [50] | 6 | Calhoun et al. [5] Chapleau et al. [6] Mueser et al. [17] Mueser et al. [18] Renard et al. [28] Rosenberg et al. [30] |
| PDS | Self-report | Foa et al. [51] | - | 2 | Picken and Tarrier [25] Steinert et al. [34] |
| PENN-PTSD | Self-report | Hammarberg [52] | - | 1 | Kennedy et al. [12] |
| PSS-I | Interview | Foa et al. [53] | - | 2 | Kilcommons and Morrison [13] Lommen and Restifo [14] |
| PTSD-I | Interview | Watson et al. [54] | - | 1 | Priebe et al. [27] |
Table 2: Assessment tools for PTSD.
▪ Prevalence of PTSD
Range of prevalence of PTSD starts from 0% to 55 %. Thirty studies found prevalence superior to 10 % (Figure 4).
Among countries which published the more studies, there is a range between 10 % and 55% in USA, between 12% and 51% in Germany and between 9% and 53% in the United Kingdom .
Only two studies found a difference of prevalence between men and women, with a higher prevalence for women. Other studies did not found this difference or did not mention it.
Discussion
We found 38 studies which explored prevalence of PTSD in SSD, that is 18 more studies than Achim et al. [18]. Prevalence of trauma exposure in SSD was generally over 80%, a rate quite similar to that reported in the general population (89.7% [21]). This seems to refute the assumption that patients with SSD have a higher trauma exposure and, conversely, is in line with the hypothesis that these patients show increase vulnerability to traumatic events [16]. Range of prevalence of PTSD was extremely wide (over 50% between the lowest value and the highest), with 30 of the 38 studies (78.9%) finding prevalence over 10%, consistent with Achim et al. findings. Even if results are heterogeneous, when we compare to general population, prevalence of PTSD in SSD remains superior. For example, in USA, prevalence of PTSD in SSD is 1, 8 to 8 times higher than in general population (general population= 6,8% [22]; SSD = 10%-55%). Contrary to general population where women are more subject to PTSD [23], we did not found differences between genders in SSD.
Many causes can explain the heterogeneity of the reported prevalence of PTSD in SSD. The first one is the heterogeneity of samples. Most studies included SSD, which mean schizophrenia, schizoaffective disorder and schizophreniform disorder. When we look at studies that separated data of schizophrenia and schizoaffective disorder, we observe that prevalence of PTSD is higher in schizoaffective disorder than it is in schizophrenia. Alvarez et al. found a prevalence of PTSD of 10.2% in schizophrenia while it was 22.2 % in schizoaffective disorder, a rate similar to bipolar disorders (21%; [24]). Other causes of heterogeneity occurred when studies included only one gender or included SSD with other comorbidities such as drug abuse. In the general population, patients with substance use disorder have higher risk of comorbid PTSD (36,6%; [25]. The only 2 studies that included SSD with substance use disorder found a very high prevalence of PTSD [26,27]. Also, the assessment of the prevalence of PTSD was made in inpatients and outpatients which can cause large variations. Indeed, recent works show the traumatic impact of psychiatric disorder and, in some cases, of psychiatric care. Several studies showed that hospitalization can cause trauma, especially seclusion and isolation [28,29]. Several authors modify criteria A of DSM definition for PTSD in order to include trauma linked to disease and to care [16,30]. When Lommen and modify the A criteria of DSM definition of PTSD and included trauma exposure linked to hospitalization and disorder, the prevalence of PTSD was estimated to 39 % while when they apply strictly DSM 4 criteria, the prevalence of PTSD dropped at 9% [16]. On the opposite, some authors deliberately excluded patients with trauma linked to care and disease [31,32]. Despite a growing literature on the traumatic impact of first psychotic episode and hospitalization, DSM5 did not include care and disorder trauma in criteria A of PTSD.
We also notice that 66 % of the studies had less than 100 patients, suggesting a majority of studies could be less representative of the SSD population, especially given the heterogeneity of this population.
Another factor of heterogeneity is the variety of tools used to assess prevalence of PTSD. Only 9 studies used the CAPS, considered as the gold standard of PTSD diagnosis [33] and only 3 used the Clinician-Administered PTSD Scale for Schizophrenia (CAPS-S) which is a modified version of the CAPS for patients with schizophrenia [34]. Besides CAPS-S and general psychiatric assessment tools (SCID, MINI), none of the tools used to assess PTSD were validated for SSD. [35] did a validity study of the PCL-5 in patients with SSD. Results showed a very high number of false positive (70.3 %), which renders the PCL an inadequate screening tool with an overrating of PTSD diagnosis [35]. Even if some modifications were made between PCL-S and PCL-5, we can speculate that the prevalence of PTSD in studies using the PCL-S might be overrated. Few screening tools were validated for patients with SSD. Moreover, most of the scales used were self-report tools, which might weaken the reliability of PTSD diagnosis. We included every study that had reported prevalence of PTSD in SSD. This can create a bias as not all of these sutdies were designed for this epidemiologic purpose. Also, we excluded 38 studies which did not report a prevalence of PTSD in SSD. Some of these studies did assess the prevalence of PTSD but in the context of broad severe mental illness and they did not provide specific data about the prevalence of PTSD in SSD.
Our review suggests that the prevalence of PTSD tends to be higher in patients with SSD than in the general population. Links between trauma and schizophrenia are still unexplained. Mueser et al elaborated an interactive model in which each group of symptoms of PTSD influences the evolution of schizophrenia, which lead to more frequent relapses and more severe symptoms [36]. Avoidance syndrome worsens schizophrenia symptoms and impairs areas of functioning, re-experience syndrome acts as stressors, over arousal syndrome increases negative symptoms and the vulnerability to retraumatization.
This review suggests that assessment of PTSD in SSD should be an important matter in everyday clinic. Impact of PTSD on SSD is not negligible, as SSD patients with comorbid PTSD tend to have more severe psychotic symptoms and are more subject to depressive and anxious symptoms [19,37–39]. Suicidal risk is increased in patients with SSD, as well as suicide attempts and substance use disorders all of which worsen the prognosis [31,40,41]. Comorbid PTSD decreases quality of life, self-worth and increases the use of medical and psychiatric care [19,42-45]. In line with this, it should be emphasize that the association between psychiatric disorders and obesity and/or diabetes constitutes a major public health concern and needs to be specifically addressed in the management of these disorders and of this comorbidity [46,47].
Despite all these clinical implications, PTSD in SSD remains under diagnosed [16,40,48-50]. One explanation could be the similarities of symptoms between PTSD and schizophrenic disorders [39,51]. Indeed, there is a certain amount of overlap between symptoms in both disorders: for instance, hallucinations are present in schizophrenia but also in some cases of PTSD, or avoidance in PTSD which can be confused with negative symptoms in schizophrenia. Also, clinicians may believe that patients with SSD cannot deliver a reliable or precise story of their trauma history, which may contribute to underdiagnose PTSD in this population. Literature suggests that patients with SSD tend to under report their traumatic experiences but are as reliable as general population [52]. Finally, Resnick et al suggests that clinicians are less willing to diagnose PTSD in SSD because there are no official therapeutic recommendations [39]. Salyers et al. tried to identify barriers in diagnosis and treatment of PTSD in patient with SSD [53]. They found that physician’s competence/ confidence and his belief that an intervention would be useful is positively correlated with the percentage of patients in which PTSD has been discussed or documented. It implies that clinicians need to be trained to improve their skills and knowledge in order to detect and treat PTSD in patients with SSD. Use of diagnosis and screening tools can help clinicians in detecting PTSD. Many studies validate PTSD assessment tools in patients with SSD. Psychometric properties of THQ, CAPS and Trauma Screening Questionnaire (TSQ) were first validate for general population but also for SSD [39,52,54-57]. Moreover, Gearon et al. (2004) validated the CAPS-S, CAPS for schizophrenia with some linguistic simplifications [34]. At last, there is promising results in treatment of PTSD in patients with SSD. Many studies confirmed efficiency of Cognitive Behavioural Therapy (CBT) to treat PTSD in SSD such as cognitive restructuration [58-60] and prolonged exposed therapy [61]. Eye Movement Desensitization and Reprocessing (EMDR) showed also good results in SSD by significantly decreasing prevalence of PTSD in SSD population and by improving PTSD symptoms, verbal auditory hallucinations, anxiety and depression without secondary effects or symptomatology exacerbation [61,62].
Conclusion
Prevalence of PTSD in patients with SSD seems to be higher than in general population. However, prevalence of trauma exposure seems similar to the general population. This suggests that patients with SSD might not be overexposed but might show an increased vulnerability to trauma. A specific meta-analysis should be to done in order to incorporate the new studies and mechanisms between trauma and schizophrenia needs to be explored. The underdiagnosis of PTSD in SSD could be improved by using validated assessment tools. Improving clinician’s knowledge and skills in PTSD in SSD could decrease patients’ distress and highly improve their quality of life.
Additional Information
Competing financial interests
The authors declare no competing financial interests.
References
- van Os J, Kapur S. Schizophrenia. Lancet 374(9690), 635-645 (2009).
- Carlsson A, Lindqvist M. Effect of chlorpromazine or haloperidol on formation of 3methoxytyramine and normetanephrine in mouse brain. Acta. Pharmacol. Toxicol. (Copenh) 20(1), 140-144 (1963).
- Weinberger DR. Implications of normal brain development for the pathogenesis of schizophrenia. Arch. Gen. Psychiatry. 44(7), 660-669 (1987).
- Howes OD, Kapur S. The Dopamine Hypothesis of Schizophrenia: Version III—The Final Common Pathway. Schizophr. Bull 35(3), 549-562 (2009).
- Zubin J, Spring B. Vulnerability--a new view of schizophrenia. J. Abnorm. Psychol.. 86(2), 103-126 (1977).
- Allen NC, Bagade S, McQueen MB, et al. Systematic meta-analyses and field synopsis of genetic association studies in schizophrenia: the SzGene database. Nat. Genet 40(7), 827-834 (2008).
- Jablensky AV, Kalaydjieva LV. Genetic epidemiology of schizophrenia: phenotypes, risk factors, and reproductive behavior. Am. J. Psychiatry 160(3), 425-429 (2003).
- Bebbington P, Wilkins S, Jones P, et al. Life events and psychosis. Initial results from the Camberwell Collaborative Psychosis Study. Br. J. Psychiatry 162(1), 72-79 (1993).
- Read J, van Os J, Morrison AP, Ross CA. Childhood trauma, psychosis and schizophrenia: a literature review with theoretical and clinical implications. Acta. Psychiatr. Scand 112(5), 330-350 (2005).
- Lardinois M, Lataster T, Mengelers R, et al. Childhood trauma and increased stress sensitivity in psychosis. Acta. Psychiatr. Scand 123(1), 28-35 (2011).
- Andrianarisoa M, Boyer L, Godin O, et al. Childhood trauma, depression and negative symptoms are independently associated with impaired quality of life in schizophrenia. Results from the national FACE-SZ cohort. Schizophr. Res (2017).
- American Psychiatric Association, American Psychiatric Association, DSM-5 Task Force. Diagnostic and statistical manual of mental disorders: DSM-5. [Internet].
- Blevins CA, Weathers FW, Witte TK. Dissociation and posttraumatic stress disorder: a latent profile analysis. J. Trauma. Stress 27(4), 388-396 (2014).
- Kostaras P, Bergiannaki J-D, Psarros C, et al. Posttraumatic stress disorder in outpatients with depression: Still a missed diagnosis. J. Trauma. Dissociation 18(2), 233-247 (2017).
- Zimmerman M, Mattia JI. Is posttraumatic stress disorder underdiagnosed in routine clinical settings? J. Nerv. Ment. Dis 187(7), 420-428 (1999).
- Lommen MJJ, Restifo K. Trauma and posttraumatic stress disorder (PTSD) in patients with schizophrenia or schizoaffective disorder. Community. Ment. Health. J 45(6), 485-496 (2009).
- Green AI, Canuso CM, Brenner MJ, et al. Detection and management of comorbidity in patients with schizophrenia. Psychiatr. Clin. North Am 26(1), 115-139 (2003).
- Achim AM, Maziade M, Raymond E, et al. How prevalent are anxiety disorders in schizophrenia? A meta-analysis and critical review on a significant association. Schizophr. Bull 37(4), 811-821 (2011).
- Fan X, Henderson DC, Nguyen DD, et al. Posttraumatic stress disorder, cognitive function and quality of life in patients with schizophrenia. Psychiatry. Res 159(1-2), 140-146 (2008).
- Pollice R, Bianchini V, Conti CM, et al. Cognitive Impairment and Perceived Stress in Schizophrenic Inpatients with Post-Traumatic Stress Disorder. European. Journal. Of. Inflammation 8(3), 211-219 (2010).
- Kilpatrick DG, Resnick HS, Milanak ME, et al. National Estimates of Exposure to Traumatic Events and PTSD Prevalence Using DSM-IV and DSM-5 Criteria. J. Trauma. Stress 26(5), 537-547 (2013).
- Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 62(6), 593-602 (2005).
- Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch. Gen. Psychiatry 52(12), 1048-1060 (1995).
- Hernandez JM, Cordova MJ, Ruzek J, et al. Presentation and prevalence of PTSD in a bipolar disorder population: a STEP-BD examination. J. Affect. Disord 150(2), 450-455 (2013).
- Gielen N, Havermans RC, Tekelenburg M, et al. Prevalence of post-traumatic stress disorder among patients with substance use disorder: it is higher than clinicians think it is. Eur. J. Psychotraumatol 3 (2012).
- Aakre JM, Brown CH, Benson KM, et al. Trauma exposure and PTSD in women with schizophrenia and coexisting substance use disorders: comparisons to women with severe depression and substance use disorders. Psychiatry. Res 220(3), 840-845 (2014).
- Gearon JS, Kaltman SI, Brown C, et al. Traumatic life events and PTSD among women with substance use disorders and schizophrenia. Psychiatr. Serv 54(4), 523-528 (2003).
- Abdelghaffar W, Ouali U, Jomli R, et al. Post - traumatic stress disorder in first episode psychosis: prevalence and related factors. Clin. Schizophr. Relat. Psychoses (2016).
- Berry K, Ford S, Jellicoe-Jones L, et al. Trauma in relation to psychosis and hospital experiences: the role of past trauma and attachment. Psychol. Psychother 88(3), 227-239 (2015).
- Picken A, Tarrier N. Trauma and comorbid posttraumatic stress disorder in individuals with schizophrenia and substance abuse. Compr. Psychiatry 52(5), 490-497 (2011).
- Pallanti S, Quercioli L, Hollander E. Social anxiety in outpatients with schizophrenia: a relevant cause of disability. Am. J. Psychiatry 161(1), 53-58 (2004).
- Steinert T, Schmid P, Bergbauer G. History of trauma in people with schizophrenia predicts need for seclusion and restraint. J. Clin. Psychiatry 67(6), 995 (2006).
- Weathers FW, Keane TM, Davidson JR. Clinician-administered PTSD scale: a review of the first ten years of research. Depress. Anxiety 13(3), 132-156 (2001).
- Gearon JS, Bellack AS, Tenhula WN. Preliminary reliability and validity of the Clinician-Administered PTSD Scale for schizophrenia. J. Consult. Clin. Psychol 72(1), 121-125 (2004).
- Steel C, Doukani A, Hardy A. The PCL as a brief screen for posttraumatic stress disorder within schizophrenia. Int. J. Psychiatry. Clin. Pract 1-3 (2017).
- Mueser KT, Rosenberg SD, Goodman LA, et al. Trauma, PTSD, and the course of severe mental illness: an interactive model. Schizophr. Res 53(1-2), 123-143 (2002).
- Braga RJ, Mendlowicz MV, Marrocos RP, et al. Anxiety disorders in outpatients with schizophrenia: prevalence and impact on the subjective quality of life. J. Psychiatr. Res 39(4), 409-414 (2005).
- Peleikis DE, Varga M, Sundet K, et al. Schizophrenia patients with and without post-traumatic stress disorder (PTSD) have different mood symptom levels but same cognitive functioning. Acta. Psychiatr. Scand, 127(6), 455-463 (2013).
- Resnick SG, Bond GR, Mueser KT. Trauma and posttraumatic stress disorder in people with schizophrenia. J. Abnorm. Psychol 112(3), 415-423 (2003).
- Álvarez M-J, Roura P, Foguet Q, et al. Posttraumatic stress disorder comorbidity and clinical implications in patients with severe mental illness. J. Nerv. Ment. Dis 200(6), 549-552 (2012).
- Tarrier N, Picken A. Co-morbid PTSD and suicidality in individuals with schizophrenia and substance and alcohol abuse. Soc. Psychiatry. Psychiatr. Epidemiol 46(11), 1079-1086 (2011).
- Calhoun PS, Bosworth HB, Stechuchak KA, et al. The impact of posttraumatic stress disorder on quality of life and health service utilization among veterans who have schizophrenia. J. Trauma. Stress. 19(3), 393-397 (2006).
- Ellick JD, Paradis CM. The effects of the September 11 World Trade Center attack on a man with a preexisting mental illness. Psychiatr. Serv 55(11), 1313-1314 (2004).
- Mueser KT, Salyers MP, Rosenberg SD, et al. Interpersonal trauma and posttraumatic stress disorder in patients with severe mental illness. Schizophr. Bull 30(1), 45-57 (2004).
- Switzer GE, Dew MA, Thompson K, et al. Posttraumatic stress disorder and service utilization among urban mental health center clients. J. Trauma. Stress 12(1), 25-39 (1999).
- Lopresti AL, Drummond PD. Obesity and psychiatric disorders: commonalities in dysregulated biological pathways and their implications for treatment. Prog. Neuropsychopharmacol. Biol. Psychiatry 45(1), 92-99 (2013).
- Martins, IJ. Early Diagnosis of Neuron Mitochondrial Dysfunction May Reverse Global Metabolic and Neurodegenerative Disease. Global. Journal. Of. Medical. Research (A) 16(1), 1-8 (2016).
- Calhoun PS, Stechuchak KM, Strauss J, et al. Interpersonal trauma, war zone exposure, and posttraumatic stress disorder among veterans with schizophrenia. Schizophr. Res 91(1-3), 210-216 (2007).
- Kilcommons AM, Morrison AP. Relationships between trauma and psychosis: an exploration of cognitive and dissociative factors. Acta. Psychiatr. Scand 112(5), 351-359 (2005).
- Mueser KT, Goodman LB, Trumbetta SL, et al. Trauma and posttraumatic stress disorder in severe mental illness. J. Consult. Clin. Psychol 66(3), 493-499 (1998).
- Seedat S, Stein MB, Oosthuizen PP, et al. Linking posttraumatic stress disorder and psychosis: a look at epidemiology, phenomenology, and treatment. J. Nerv. Ment. Dis 191(10), 675-681 (2003).
- Goodman LA, Thompson KM, Weinfurt K, et al. Reliability of reports of violent victimization and posttraumatic stress disorder among men and women with serious mental illness. J. Trauma. Stress. 12(4), 587-599 (1999).
- Salyers MP, Evans LJ, Bond GR, et al. Barriers to assessment and treatment of posttraumatic stress disorder and other trauma-related problems in people with severe mental illness: clinician perspectives. Community. Ment. Health. J 40(1), 17-31 (2004).
- Blake DD, Weathers FW, Nagy LM, et al. The development of a Clinician-Administered PTSD Scale. J. Trauma. Stress 8(1), 75-90 (1995).
- de Bont PAJM, van den Berg DPG, van der Vleugel BM, et al. Predictive validity of the Trauma Screening Questionnaire in detecting post-traumatic stress disorder in patients with psychotic disorders. Br. J .Psychiatry 206(5), 408-416 (2015).
- Grubaugh AL, Elhai JD, Cusack KJ, et al. Screening for PTSD in public-sector mental health settings: the diagnostic utility of the PTSD checklist. Depress. Anxiety 24(2), 124-129 (2007).
- Mueser KT, Salyers MP, Rosenberg SD, et al. Psychometric evaluation of trauma and posttraumatic stress disorder assessments in persons with severe mental illness. Psychol. Assess 13(1), 110-117 (2001).
- Frueh BC, Grubaugh AL, Cusack KJ, et al. Exposure-based cognitive-behavioral treatment of PTSD in adults with schizophrenia or schizoaffective disorder: a pilot study. J. Anxiety. Disord 23(5), 665-675 (2009).
- Marcello SC, Hilton-Lerro K, Mueser KT. Cognitive Behavioral Therapy for Posttraumatic Stress Disorder in Persons With Psychotic Disorders. Clinical. Case. Studies 8(6), 438-453 (2009).
- Mueser KT, Gottlieb JD, Xie H, et al. Evaluation of cognitive restructuring for post-traumatic stress disorder in people with severe mental illness. Br. J. Psychiatry 206(6), 501-508 (2015).
- de Bont PAJM, van Minnen A, de Jongh A. Treating PTSD in patients with psychosis: a within-group controlled feasibility study examining the efficacy and safety of evidence-based PE and EMDR protocols. Behav. Ther 44(4), 717-730 (2013).
- van den Berg DPG, van der Gaag M. Treating trauma in psychosis with EMDR: a pilot study. J. Behav. Ther. Exp. Psychiatry 43(1), 664-671 (2012).